

| Table 1 | |
| Metabolic: | Juvenile osteoporosis |
| Inflammatory: | Ankylosing Spondylitis Sero-negative Arthritis |
| Neoplasm: | Osteoid osteoma |
| Congenital: | L5-S1 facet Hypoplasia |
| Developmental: | Lumbar Scheurmann's |
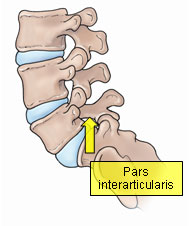
| Trauma: | Pars interarticularis |
Adolescent back pain has been reported to affect more than 50% of school age patients. Parents are often confounded by the severity of the complaints and yet their teenager continues in sports or other extracurricular activities. After months of complaints and minimal relief of symptoms with anti-inflammatory drugs, the family will seek an evaluation.
The adolescent with lumbar back pain may have multiple reasons other than overuse or "growing pains" for the discomfort. (Table 1)
The clinical examination provides information about the location of the pain, muscle spasm, lumbar spine range of motion, hamstring muscle tightness, muscle strength in the legs, reflexes, and sensation in the legs.
X-ray studies may discount several of the potential diagnoses and direct the physician to propose the diagnosis of a pars interarticularis stress injury or fracture.
The pars interarticularis is a portion of the lumbar spine that joins the upper and lower joints together. The pars is normal in the vast majority of children.
After approximately 8 YOA, certain patients begin to experience abnormal growth and development of this particular region in the bone. A genetic weakness to the bone has only been established in certain ethnic groups such as Alaskan Indians. It does appear that certain athletic activities or injuries (gymnastics, heavy weight lifting) may result in problems in susceptible individuals.
There are three stages of injury to the pars interarticularis:
Stress reaction or injury may occur when the bone experiences excessive wear and tear from activities of daily living, sports, or a fall. The symptoms may include lumbar pain, stiffness, and hamstring muscle tightness. X-rays will not reveal any abnormality. A bone scan will demonstrate the inflammation in the pars. Treatment consists of relieving the pain and restoring spinal flexibility. After several months, the majority of patients resume most activities.
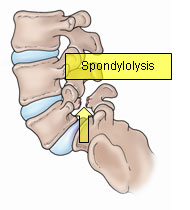
If the pars "cracks" or fractures, the condition is called Spondylolysis. The x-ray confirms the bony abnormality. Treatment is customized based on the severity of symptoms. Anti-inflammatory drugs, physical therapy, brace wear, and activity modifications will be considered. core exercisesPrior to a release to activities after the pain resolves, a course of truncal core muscle strengthening (pilates or yoga) may be prescribed to condition the muscles and minimize reinjury.
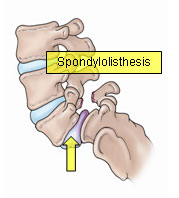
If the fracture gap at the pars widens, then the condition is called Spondylolisthesis. Widening of the gap leads to the fifth lumbar vertebra shifting forward on the part of the pelvic bone called the sacrum. Standing lateral spine x-rays are measured to determine the amount of forward slippage.
Treatment is prescribed to decrease any acute spasm and restore spinal flexibility. One of the mainstays of physical therapy treatment is to perform truncal core strengthening exercises. The therapist will caution the patient on avoiding hyperextension maneuvers and excessive abdominal "crunches".
Prognosis is affected by the amount of slippage. In general, most patients with less than 50% slippage fend to fare well through adolescence. With slippage of 50% or greater, the potential for additional slippage with growth and aging is greater. The small numbers of patients who do not respond to conservative medical management are evaluated for a spinal fusion.
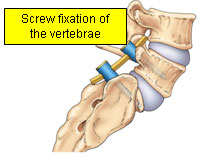
If the pain, spasm, or slippage increases, then the surgeon will discuss several potential surgical options. For a majority of children, fusing the 5th lumbar vertebra to the sacrum is the first choice. The fusion involves removing the loose bony fragments and placing bone graft in such a manner that will lead to the successful "gluing together" of the two vertebra.
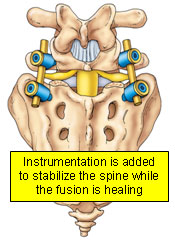
The patient is restricted postoperatively with a cast or brace until healing is complete. In older patients the alignment of the two vertebra may benefit from the addition of bone screws during the healing process.
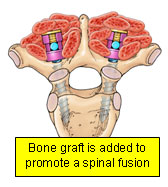
Bone graft is still added to promote a fusion that may take up to three to six months to heal completely. After a successful fusion most athletic activites can be enjoyed once again.