


Scoliosis in patients between 10 and 18 years of age is termed adolescent scoliosis and can be due to many causes. By far the most common type of scoliosis in the adolescent period is one in which the cause is not known and is called idiopathic or adolescent idiopathic scoliosis (AIS). Although significant ongoing research continues in this area, including the genetic basis for AIS, there are no identifiable causes for this condition today. Despite this, we currently have accurate methods to determine the risk for curve progression of scoliosis and good methods of treatment. Learn more about this topic in the Education Resource Center.
There are significant efforts being made toward identifying the cause of AIS, but to date there are no well accepted causes for this particular type of scoliosis. The vast majority of patients are otherwise healthy and have no previous medical history. There are many theories about the cause of AIS including hormonal imbalance, asymmetric growth, and muscle imbalance. Approximately 30% of AIS patients have some family history of scoliosis, and therefore there seems to be a genetic connection. Many Scoliosis Research Society members are working to identify the genes that cause AIS, and this knowledge continues to expand at a rapid pace. Most likely, there will be many genes associated with scoliosis and each may be helpful in detecting scoliosis and determining the risk for progression of the curve.
Adolescent idiopathic scoliosis generally does not result in pain or neurologic symptoms. The curve of the spine does not put pressure on organs, including the lung or heart, and symptoms such as shortness of breath are not seen with AIS. When scoliosis begins in adolescence, patients may have some back pain, typically in the low back area. Although it is often associated with scoliosis, it is generally felt that the curvature does not result in pain. Low back pain is not uncommon in adolescents in general. Many teens experience back pain due to participating in a large number of activities without having good core abdominal and back strength, as well as flexibility of the hamstrings.
Adolescent idiopathic scoliosis generally does not result in pain or neurologic problems. If these symptoms occur, further evaluation and testing may be necessary to include an MRI, CAT scan or Bone scan.
There are many visible symptoms associated with adolescent idiopathic scoliosis. Depending on the curve pattern and the size or magnitude of the curve, scoliosis may be barely seen or it may have significant visible symptoms. One of the most common is shoulder height asymmetry, in which one shoulder appears higher than the other (see figure 1). A shift of the body to the right or the left can occur especially when there is an single curve in the thoracic (chest-part) or the lumbar (lower back) of the spine without a second curve to help balance the patient. This is often seen as some waistline asymmetry in which one hip appears to be higher than the other and may result in one leg appearing taller than the other (see figure 2). A prominence on the back or a rib hump secondary to the rotational aspect of the scoliosis is the most visible sign of scoliosis (see figure 3).
Patients with AIS generally have a normal appearance when viewed from the side. In general, there are no neurologic abnormalities such as weakness or changes in a patients feeling in the upper or lower extremities (see figure 4).




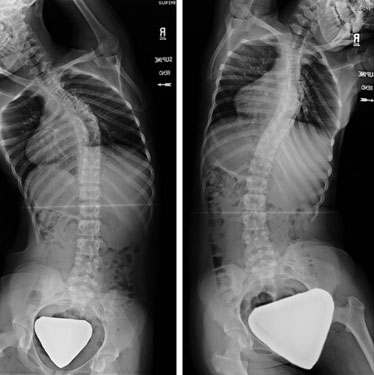
The typical radiographic images that are obtained to define scoliosis include a standing X-ray of the entire spine looking both from the back (PA radiograph), as well as from the side (lateral radiograph) (see figure 1). These radiographs are often done with lead shields to protect the patient while allowing for a clear view of the spine. Your physician will be able to measure the radiographs to determine your curves magnitude, which is measured in degrees using the Cobb method (see figure 2). A straight spine has a curve of 0º, any curve greater than 10º is considered scoliosis. Between 0º and 10º is considered a curvature which is not true scoliosis. The way a patient stands at the time of an X-ray or many other factors can cause a slight curvature. The lateral radiograph is used to determine the thoracic kyphosis (or roundback appearance) and the amount of lumbar lordosis (swayback).


Further radiographs can be performed to determine the flexibility of the curvature (how much it straightens). These flexibility radiographs can be done several ways. X-rays can be taken in which the patient lays on the table and bends to the right and then to the left (see figure 3). Traction films are taken with the patient's arms and legs pulled to stretch the spine out. A fulcrum- bend radiograph is taken with a padded roll placed at the apex of the curve to improve the curve correction. These radiographs are most often taken in the planning of surgical treatments.
When bracing treatment is started, radiographs are usually performed with the brace on to ensure that the brace is effective in achieving some correction of the curve(s) (see figure 4). When bracing is use to make a correction X-rays are often used to determine progress. These X-rays can be taken either in the brace or out of the brace depending on the preference of the physician.
A magnetic resonance imaging (MRI) study of the spine is not routinely obtained for patients with AIS. The MRI is specifically used to review other things in addition to the bones of the spine, for instance to view the spinal cord to ensure there are no abnormalities. An MRI is usually ordered if your physician finds some subtle neurologic abnormalities on physical examination, if there is significant pain associated with the scoliosis or if the radiographs demonstrate an "atypical" curve pattern. The likelihood of having something abnormal on the MRI is very small but would require further evaluation with a neurosurgeon if abnormalities are seen.
Treatment of adolescent idiopathic scoliosis falls into three main categories (observation, bracing and surgery), and is based on the risk of curve progression. In general, AIS curves progress in two ways: 1. during the rapid growth period of the patient, and 2. into adulthood if the curves are relatively large.
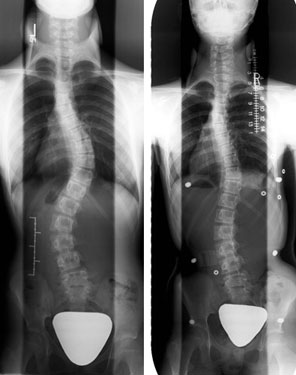
Since scoliosis gets larger during rapid growth, the potential for growth is evaluated taking into consideration the patient's age, the status of whether females have had their first menstrual period, as well as radiographic parameters. In general, girls grow until 14 years of age, while boys grow until 16 years of age. Girls grow very rapidly until their first menstrual period, and then their growth generally slows down, but they continue to grow until 18 months to 2 years after their first menstrual period. Radiographs of the spine and pelvis are also used to determine growth. The Risser grading system (Figure 1) is often used to determine a child's skeletal maturity (how much growth is left) on the pelvis, which correlates with how much spine growth is left. The Risser grading system rates a child's' skeletal maturity on a scale of 0 to 5. Patients who are Risser 0 and 1 are growing rapidly, while patients who are 4 and 5 have stopped growing. Generally patients who are being treated in a scoliosis clinic will have their height measured at each visit to help determine growth potential. An Xray can also be performed of a patient's hand. This Xray can examine the growth plates (epiphysis) of the fingers and hand bones to evaluate a child's skeletal maturity and potential for further growth.
Large curves are also more likely to progress or worsen. Curves greater than 45º in patients who are growing, or curves greater than 50º in patients who are done growing will continue to slowly progress over time. This is a general rule and there are exceptions based on multiple factors which your physician will determine.

Observation is generally for patients whose curves are less than 25º who are still growing, or for curves less than 50º in patients who have completed their growth.
Alternative treatments to prevent curve progression or prevent further curve progression such as chiropractic medicine, physical therapy, yoga, etc. have not demonstrated any scientific value in the treatment of scoliosis. However, these and other methods can be utilized if they provide some physical benefit to the patient such as core strengthening, symptom relief, etc. These should not, however, be utilized to formally treat the curvature in hopes of improving the scoliosis.
Bracing is for patients with curves that measure between 25º and 40º during their growth phase. The goal of the brace is to prevent the curve from getting bigger. This is accomplished by correcting the curve while the patient is in the brace so that the curve does not progress with time. Once the brace is discontinued, the best one hopes for is to not have any curve progression, and to remain at the curve magnitude present when the brace was started. For example, a young girl who is 11 years of age who is a Risser 0, with a curve measuring 30º, will be prescribed the brace and will wear the brace until growth of the spine has stopped (Risser 4 or 5, two years after the menstrual period). For that particular patient the best he/she can hope for is to prevent progression and end treatment with a 30 degree curve. Even if slight curve progression occurs despite wearing the brace, surgical treatment is not necessary as long as the curve remains below 45 degrees at the end of growth. There are several types of braces available but all of them work in the same fashion. All braces are worn under the clothes and cannot be seen by others.
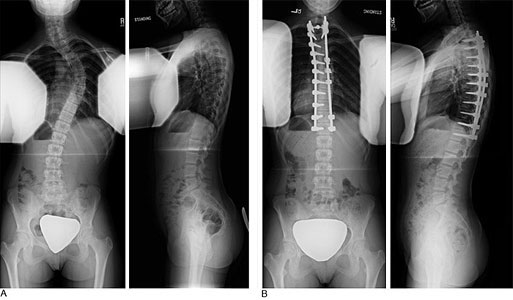
Surgical treatment is used for patients whose curves are greater than 45º while still growing or greater than 50 º when growth has stopped. The goal of surgical treatment is two-fold: First, to prevent curve progression and secondly to obtain some curve correction. Surgical treatment today utilizes metal implants which are attached to the spine, and then connected to a single rod or two rods. Implants are used to correct the spine and hold the spine in the corrected position until the spine segments which have been operated on are fused as one bone. The surgery can be performed from the back of the spine (posterior approach) (Figure 2) through a straight incision along the midline of the back or through the front of the spine (anterior approach) (Figure 3). Although there are advantages and disadvantages to both approaches, the posterior approach is utilized most often in the treatment of AIS and can be utilized for all curve types. The anterior approach is an option when a single thoracic curve or a single lumbar curve is being treated. Many factors go into the decision as to the surgical approach and your doctor will review the options and choose the best approach for you.
Following surgical treatment, no external bracing or casts are used. The hospital stay is generally between 5 and 7 days. The patient can perform regular daily activities and generally returns to school in 3-4 weeks. Depending on the activities of the patient, full participation is allowed between 3 and 6 months after surgery.

In general, AIS does not cause symptoms and should not restrict patients with respect to physical activities. For those patients who have mild scoliosis and who are being watched by their physician, all activities can be performed without any restriction or risk for injury. For those patients who are undergoing brace treatment, all physical activities are allowed while the brace is not being worn. For patients who have surgical treatment, your surgeon will provide you with information as to what activities are allowed following treatment.