


Infantile idiopathic scoliosis is classically defined as scoliosis that is first diagnosed between birth and 3 years of age. This category comprises about 1% of all idiopathic scoliosis in children. 60% of patients are males. The etiology of the scoliosis remains unknown despite interest in 2 theories. The intra-uterine molding theory suggests that the spine is bent at the time of birth and worsens with growth. The post delivery theory suggests that placing the infant their back will lead to flattening of the skull and scoliosis. Due to the fact that more progressive curves occur in Europe than in the U.S., a genetic cause has been postulated but still unproven.
The diagnosis of idiopathic infantile scoliosis is based on the age of onset, the absence of any other spinal cord problems, the location of the curve, findings on physical examination, and x-rays. The characteristic finding on physical examination is that the curve is typically between the shoulder blades or in the thoracic region of the spine and the spine curves to the left. The MRI is normal in infantile idiopathic scoliosis.
Infantile curves that reach 30 degrees tend to continue to worsen without treatment. In addition to the degree of scoliosis, the Mehta rib vertebral angle degree difference has greater prognostic value. The Mehta angle is determined by identifying the vertebra in the apex or middle of the curve and measuring the difference in the angle of each rib attaching to the vertebra (Figure 1). A Mehta difference of 20 degrees or less is associated with a non progressive or resolving curve in most cases. Girls with right sided curves tend to have more progressive curves than other infants. 25 year follow up studies demonstrate a normal quality of life in patients with non progressive infantile scoliosis.
Observation is usually the first method of treatment for a young child with a spinal deformity. Rates of spontaneous resolution of infantile scoliosis have been reported from 18% to 92%. This high degree of variability likely reflects a debate about which curves represent real scoliosis, and which are simply normal developmental conditions. The physician will first need to determine if the curvature is progressing or worsening. Some children will have a curvature of their spine that is stable and unchanging, whereas other children will have a curve that relentlessly progresses. Just because the pediatric spine surgeon is "observing" your child does not mean that he/she is not treating them. Your pediatric spine surgeon will probably want to see your child every four to six months and have new x-rays made. They will then measure the curves and compare them with the previously made films. It is ideal to have all of the x-rays done at the pediatric spine surgeon's office so that he/she can have similar types of films for comparison. The doctor will probably continue to observe your child's curves as long as there is no drastic increase in the size of the curve. Fortunately, in many cases, curves do improve or resolve spontaneously. However, if your pediatric spine surgeon documents progression of the curve, a different form of treatment will need to be instituted.
If the curve is progressive, and your child is still growing, the doctor may want to place your child in a cast or brace. This is contingent upon the flexibility of the curve, as determined by x-rays. If the curve is rigid and does not correct (get smaller) on the bending films, a brace will do little good. Rarely does a brace permanently correct scoliosis; instead the goal of bracing is to allow the child to grow before a more definitive procedure (surgery) is done. It must be re-emphasized that the purpose of the brace is to slow the inevitable progression of the curve, not to correct the curve.
The brace that your doctor prescribes depends on your child's age and the center you visit. There are several types of braces, which typically have the same success rates, but your doctor will select one based on his/her experience with the different devices. The Kallabis brace has several straps that are applied over the shoulder and bend the child in the opposite direction of the curve (Figure 1). The Wilmington brace is a custom-molded thoracolumbosacral orthosis that has molds to push and correct the curve (Figure 2). The Boston brace is similar, but uses pads inside the brace to push the curve. The Milwaukee brace, one of the first braces developed for scoliosis treatment, is less popular today due to its design, which can include an extension to the chin. Your doctor will probably recommend that your child wear the brace fulltime. Braces are generally removed for bathing and special occasions. As your child grows, new braces will need to be fabricated, approximately every twelve to eighteen months.
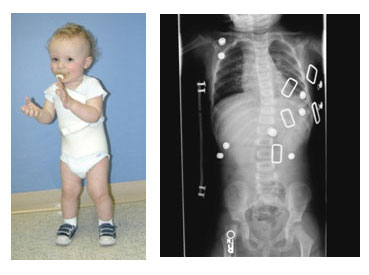


If the curve is progressive, serial casting (Figure 1) can be used to partially correct the deformity before beginning bracing. A cast can be considered a full-time brace which cannot be removed. Many parents prefer casting because it eliminates the problems of compliance and the difficulties of donning braces in uncooperative young children.
Casting can become a definitive method of management. Research in the United Kingdom indicates that treating non-congenital scoliosis with serial casts beginning in children at 12 months of age with an average curve of 32o in some cases have their scoliosis reduced to up to <10o at maturity. Patients starting treatment at 18 months or later, with larger curves averaging 52o, achieve less correction, but their deformities can be maintained at a similar degree of magnitude.
The goal of casting in children under 2 years of age is curing the scoliosis. This requires cast changes under anesthesia every 2-3 months (minimum 5 casts) with the goal of achieving a straight spine. Despite the extensive casting, a brace will still be needed after the casting treatment. Older children demonstrating "recurrence" can be re-casted for four months to re-correct the deformity before continuing with brace management.
An operation is sometimes necessary to address spinal deformity in the young child, and the decision to do this is based on many factors. If the child's curve has shown progression despite bracing or casting, something different will need to be done (Figure 1). The dilemma faced by the surgeon is how to stop the progression of a curve without adversely affecting future growth. Sometimes this is unavoidable, as most operations work by stopping abnormal spinal growth in a procedure called spinal fusion.


Spinal fusion is a procedure performed to stop growth of the spine. It can be done from the back (posterior) or through the chest (anterior) or both. The joints of the spine are removed, and a bone graft is placed; when the bone heals there will be a fusion mass, or one solid piece of bone. The goal is for the many vertebrae of the spine to become one segment and to stop growing crooked. In situ fusion means that the curve will be fused "where it is" with little or no correction of the spine. Sometimes instrumentation (rods, hooks, and screws) may be placed to help straighten the spine slightly and act as an internal brace for the bone graft that will form the fusion mass. Usually instrumentation is not used in young children and the child may need to wear a brace or cast following the operation.
The goal of an in situ spinal fusion is to address the problem early, before it becomes a serious deformity. For example, if a pediatric spine surgeon sees a child with a 40o curve that has a poor prognosis (high chance to progress); he/she may elect to perform a limited spinal fusion to prevent the curve from getting any bigger. It is generally a safer procedure than the surgeries that correct the curvature of the spine. The results of a procedure to correct the curve at a young age can be unpredictable, as continued growth of the spine in other areas can cause the curve to progress or rotate (twist around).
Most operations that address spinal deformity in the young child work by stopping growth. This may have unfavorable effects on growth of the thorax (chest), lung development, and size of the trunk. The theory of the growing rod operation is to allow for continued controlled growth of the spine. This is done through the back of the spine. In general, the curve is spanned by one or two rods under the skin to avoid damaging the growth tissues of the spine. The rods are then attached to the spine above and below the curve with hooks or screws. The curve can usually be corrected by fifty percent at the time of the first operation. The child then returns every six months to have the rods "lengthened" approximately one centimeter to keep up with the child's growth. This is usually an outpatient procedure and is performed through a small incision. Most children will have to wear a brace to protect the instrumentation. When the child becomes older and the spine has grown, the doctor will remove the instrumentation and perform a formal spinal fusion operation. In the past, this procedure had a very high complication rate, most of which were related to the instrumentation (hook dislodgement, rod breakage). Newer techniques are more promising, such as rods that are expanded with a magnet placed on the patient's back in the outpatient clinic and do not require scheduled expansions in the operating room. However, treatment with growing rods remains a long and difficult therapy for the child.
Definitive spinal fusion is performed to stop growth of the spine and thus achieve permanent correction. This treatment becomes appropriate when the patient has achieved sufficient spinal length and thoracic width and depth. It is important to determine that the growth stoppage will not in itself produce thoracic insufficiency. Timing of the procedure is controversial, but in general, patients who have reached age 10 have completed the greatest part of their thoracic growth, and thus are candidates for definitive fusion to finish their scoliosis treatment.
Posterior fusion provides permanent stabilization in the corrected position and is achieved by removing the joints between the vertebrae to be fused. These are usually all the vertebrae which are involved in the curve. Bone graft - either from the pelvis, ribs, or from the bone bank (allograft) - is placed in each joint space which has been removed. Over time (4-6 months), the graft adheres to the vertebral bone, and the operated portion of the spine heals into a solid block of bone which cannot bend, thus eliminating further progression of the curve. Typically in a child who has reached an appropriate age for definitive fusion, instrumentation will also be placed when the fusion is performed. The instrumentation rigidly fixes the spine internally, so that the corrected position is carefully preserved while the fusion takes place over the 4-6 month period. This rigid fixation is achieved by screws, hooks, and wires ("anchors") attached to the spine, usually at multiple sites along the curve, and then rods are attached to the anchors to stiffen the entire area. Depending on the flexibility of the curve and any preceding treatment (such as traction), there may be additional correction of the deformity achieved by the application of the instrumentation. However, the primary goal of the surgery is to stop the curve from progressing further, resulting in definitive stabilization. Additional correction is an added benefit but not the primary concern. Often the patient does not need a cast or brace if the internal instrumentation is felt to be adequate at the time of surgery.
Depending on the surgeon's determination of how much growth the patient might have remaining, an anterior (front) fusion of the spine may also be appropriate. This is done either through an incision in the patient's side or rib cage, or through small incisions between the ribs, aided by a camera (thoracoscopic fusion). This will prevent curve progression after posterior (rear) fusion due to continued growth of the vertebrae. Known as the "crankshaft phenomenon", curves sometimes continue to grow by rotating around the original surgical fusion. This is known to happen when children under the age of ten undergo fusion surgery and can be prevented by performing an anterior fusion at the same time (or shortly before or after) the definitive posterior operation.
The decision to undergo the additional surgery required to prevent crankshaft curve progression is dependent on the age of the child at the time surgery is selected. Delaying definitive surgery is the best option if that delay can be accomplished while maintaining control of the curve by non-operative means.
Curves that decrease with observation or bracing are likely to remain dormant through the remaining growth spurts. Progressive curves that are treated surgically require close follow up through adulthood.