


Juvenile idiopathic scoliosis is classically defined as scoliosis that is first diagnosed between the ages of 4 and 10. This category comprises about 10% to 15% of all idiopathic scoliosis in children. At the younger end of the spectrum, boys are affected slightly more than girls and the curve is often left-sided. Towards the upper end of the age spectrum, the condition is more like adolescent idiopathic scoliosis, with a predominance of girls and right-sided curves.
Just as described for infantile scoliosis, your pediatric spine surgeon may choose to order an MRI. This decision is based on the presentation of the curve, findings on physical examination, and radiographic features. As a rule of thumb, approximately 20% of children who are younger than 10 and who have a curve greater than 20? will have an underlying spinal condition. There is a particularly high incidence of Arnold-Chiari malformation (in which the brainstem is lower than normal) and syringomyelia (cyst in the spinal cord) associated with curves under 10 yoa, which might be detected on an MRI of the entire spine. (Figure 1) If something is seen on the MRI that could be causing your child's scoliosis, your doctor will probably refer you to a pediatric neurosurgeon and the condition will be reclassified as a neuromuscular scoliosis. On occasion, a neurosurgical intervention may help correct the neuromuscular curvature.
Juvenile curves that reach 30o tend to continue to worsen without treatment. Bracing is often used to manage these curves, but nearly 95% of children in the juvenile age range go on to require surgical treatment.
Observation is usually the first method of treatment for a young child with a spinal deformity. The physician will first need to determine if the curvature is progressing--that is, getting worse. Some children will have a curvature of their spine that is stable and unchanging, whereas other children will have a curve that relentlessly progresses. During this period of time, not only will your child's doctor look for changes in the curve, but they will probably order some special tests to evaluate further the child's condition and have you see some other doctors. These tests may include an MRI study or a CT study. Your child may be referred to other specialists, such as a geneticist, cardiologist, or pulmonologist to make sure there are no other problems in other parts of the body.
Your pediatric spine surgeon will probably want to see your child every four to six months and have new front- and side-view X-rays made. They will then measure the curves and compare them with the previously made films. The doctor will probably continue to observe your child's curves as long as there is no drastic increase in the size of the curve. In some rare cases, the curve improves or even resolves (as in infantile scoliosis). If your pediatric spine surgeon documents progression of the curve, though, a different form of treatment will need to be instituted. He/she will probably want to obtain bending radiographs of the spine to assess flexibility and help determine the next course of treatment.
The underarm brace that your doctor prescribes may depend on your child's age and the center you visit. There are several types of braces, they typically have the same success rates, but your doctor will select one based on his/her experience with the different devices. The Wilmington brace is a custom-molded thoracolumbosacral orthosis that has molds to push and correct the curve (Figure 2). The Boston brace is similar, but uses pads inside the brace to push the curve (Figure 3). The Milwaukee brace, one of the first braces developed for scoliosis treatment, is less popular today due to its design. Your doctor will probably recommend that your child wear the brace fulltime. Some lumbar and thoracolumbar curves will be treated by a part time or night time brace. The Charleston and Providence braces are prescribed for eight to twelve hours a day, typically only during the hours of sleep. Braces are generally removed for bathing and special occasions. As your child grows, new braces will need to be fabricated, approximately every twelve to eighteen months.



Braces may not be effective in every child for various reasons. The curve may be stiff and resistant to correction. Braces also have a more difficult time controlling kyphosis (round back) and lordosis (sway back). Since most braces work on the curve via the pressure they exert on the rib cage, concern exists over the effect that the brace has on the rib cage and the subsequent development of the lungs. Children with reflux, feeding tubes, and colostomies may have difficulty wearing a brace, but modifications can be made.

Serial casting can be used to delay the need for bracing by correcting the deformity sufficiently to allow bracing to then be re-instituted. Since a cast can be considered a full-time brace which cannot be removed, many parents find it preferable to braces, eliminating the problems of compliance and the difficulties of donning braces in uncooperative young children.
A few centers treat children with a body cast as a form of a brace (Figure 1). Placement of the cast on the child may require general anesthesia to increase flexibility of the curve and make the child more comfortable during the application. The cast is generally changed every six months, usually under an anesthetic. Casting can offer superior curve management, at the cost of its inconvenience (cannot be removed for bathing).
Treatment for patients with a progressive deformity who are not a candidate for bracing or casting can be more difficult, for example those with weakness, skin or chest wall intolerance, mental retardation, or with large and stiff curves that do not correct much during serial casting. In these instances, halo-gravity traction is a method to achieve deformity correction, and indirectly, improve respiratory mechanics. The traction method of treatment has recently regained popularity in some centers.
A halo (metal ring around the head) is applied under general anesthesia. Multiple pins attach the ring to the patient's skull. The halo is not painful and is well tolerated after the patient becomes accustomed to its presence. Traction is applied the following day with the use of ropes, pulleys, and weights or springs that can be applied to the child's bed or a wheelchair. Some patients can be treated as outpatients if the family is comfortable. The children are followed with serial X-rays after successive increases in the weight of the traction. Once the spine has shown the maximal amount of improvement, your surgeon will decide the next course of treatment which is usually surgical fusion of the scoliotic curve.
An operation is sometimes necessary to address spinal deformity in the young child, and the decision to do these procedures is based on many factors. If the child's curve has shown progression despite bracing or casting, something will need to be done. The dilemma faced by the surgeon is how to stop the progression of a curve without adversely affecting future growth. Sometimes this is unavoidable, as most operations work by stopping abnormal spinal growth in a procedure called spinal fusion.
Spinal fusion is a procedure performed to stop growth of the spine. It can be done from the back (posterior) or through the chest (anterior). The joints of the spine are removed, and a bone graft is placed; when the bone heals there will be a fusion mass, or one solid piece of bone. The goal is for the many vertebrae of the spine to become one segment and stop growing crooked. In situ fusion means that the curve will be fused "where it is" with little or no correction of the spine. Sometimes instrumentation (rods, hooks, and screws) may be placed to help straighten the spine slightly and act as an internal brace for the bone graft that will form the fusion mass. When implants are not used, usually in young children, the child may need to wear a brace following the operation.
The goal of an in situ spinal fusion is to address the problem early, before it becomes a serious deformity. For example, if a pediatric spine surgeon sees a child with a 40o curve that has a poor prognosis (high chance to progress), he/she may elect to perform a limited spinal fusion to prevent the curve from getting any bigger. It is generally a safer procedure than those that correct the curvature of the spine. The results of a procedure to correct the curve at a young age can be unpredictable, as continued growth of the spine in other areas can cause the curve to progress or rotate (twist around).
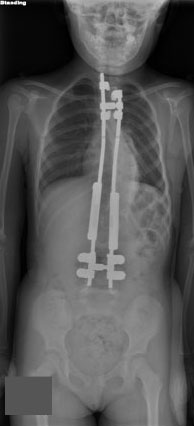
Most operations that address spinal deformity in the young child work by stopping growth. This may have unfavorable effects on growth of the thorax, lung development, and size of the trunk. The theory of the growing rod operation is to allow for continued controlled growth of the spine. This is done through the back of the spine. In general, the curve is spanned by one or two rods under the skin to avoid damaging the growth tissues of the spine. The rods are then attached to the spine above and below the curve with hooks or screws. The curve can usually be corrected by fifty percent at the time of the first operation (Figure 1). The child then returns every six months to have the rods "lengthened" approximately one centimeter to keep up with the child's growth. This is usually an outpatient procedure performed through a small incision. Most children will have to wear a brace to protect the instrumentation. When the child becomes older and the spine has grown, the doctor will remove the instrumentation and perform a formal spinal fusion operation. In the past, this procedure had a very high complication rate, most of which were related to the instrumentation (hook dislodgement, rod breakage). Newer techniques are more promising, such as rods that are expanded with a magnet placed on the patient's back in the outpatient clinic and do not require scheduled expansions in the operating room. However, treatment with growing rods remains a long and difficult therapy for the child.

Definitive spinal fusion is performed to stop growth of the spine and thus achieve permanent correction. This treatment becomes appropriate when the patient has achieved sufficient spinal length and thoracic width and depth that the growth stoppage will not in itself produce thoracic insufficiency. When exactly it might be appropriate to proceed may be controversial, but in general, patients who have reached age 10 have completed the greatest part of their thoracic growth, and thus are candidates for definitive fusion to finish their scoliosis treatment.
Posterior fusion provides permanent stabilization in the corrected position and is achieved by removing the joints between the vertebrae to be fused, usually all the vertebrae which are involved in the curve. Bone graft - either from the pelvis, ribs, or from the bone bank (allograft) - is placed in each joint space which has been removed. Over time (4-6 months), the graft incorporates to the vertebral bone, and the operated portion of the spine heals into a solid block of bone which cannot bend, thus eliminating further progression of the curve. Typically in a child who has reached an appropriate age for definitive fusion, instrumentation will also be placed when the fusion is performed. The instrumentation rigidly fixes the spine internally, so that the corrected position is carefully preserved while the fusion takes place over the 4-6 month period. This rigid fixation is achieved by screws, hooks, and wires ("anchors") attached to the spine, usually at multiple sites along the curve, and then rods are attached to the anchors to stiffen the entire area. Depending on the flexibility of the curve and any preceding treatment (such as traction), there may be additional correction of the deformity achieved by the application of the instrumentation. However, the primary goal of the surgery is to stop the curve from progressing further, and thus be the definitive stabilization - additional correction is an added benefit but not the primary concern. Often the patient does not need any further external immobilization (cast or brace) if the internal fixation device is felt to be adequate at the time of surgery.
Depending on the surgeon's determination of how much growth the patient might have remaining, an anterior (front) fusion of the spine may also be appropriate. This will prevent curve progression after posterior (rear) fusion due to continued growth of the vertebrae. Known as the "crankshaft phenomenon", curves sometimes continue to grow by rotating around the original surgical fusion. This is known to happen when children under the age of ten undergo fusion surgery and can be prevented by performing an anterior fusion at the same time (or shortly before or after) the definitive posterior operation.
Obviously the additional surgery required to prevent crankshaft curve progression is best not done at all if it is not necessary, the decision being dependent on the age of the child at the time surgery is selected. Delaying definitive surgery is the best option if that delay can be accomplished while maintaining control of the curve by non-operative means.
Several studies have demonstrated a favorable long term outcome to curves treated nonoperatively if the residual curve measures less than forty degrees and there is minimal truncal imbalance.
Similar studies have demonstrated a favorable outcome with individuals who underwent a surgical fusion that left two or more motion segments free at the bottom of the spine.
Long term studies show that large curves of sixty degrees or more have a distinct potential for progression over the ensuing 3-4 decades and that symptoms may develop and require treatment.