

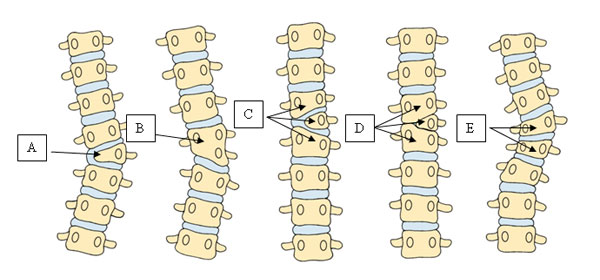
 Figure 1: Complex congenital spine deformity.
Figure 1: Complex congenital spine deformity.The term "congenital scoliosis" refers to a spinal deformity caused by vertebrae that are not properly formed. This occurs very early in development; in the first six weeks of embryonic formation. Congenital scoliosis does not seem to run in families. Genetic studies to date have not yielded much evidence that this condition can be inherited. Although congenital scoliosis is often discovered during the infant or toddler period, in some children it does not diagnosed until their adolescent years.
Pediatric spine surgeons describe congenital spinal anomalies based on which part of the vertebra is malformed or connected. Depending on the structure of the anomaly, the child may exhibit scoliosis (a curve to the right or left), kyphosis (round back), or lordosis (sway back). However, not all congenital anomalies fit neatly into these categories. There are often elements of more than one deformity, particularly scoliosis and kyphosis occurring together (Figure1).
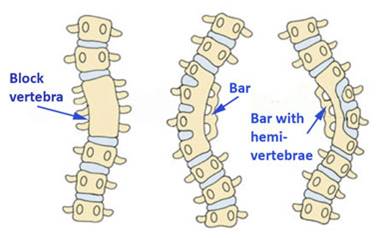
Pediatric spine surgeons may refer to the spine anomaly as a "failure of segmentation." This means that one or more vertebrae are abnormally connected together on one side. This connection will slow growth on that side of the spine. Unopposed growth on one side with slowed growth on the other leads to a spinal deformity. "Failure of formation," the most common type of congenital problem, means that the normal shape of the vertebra is disrupted (Figure 2). "Failure of segmentation" means that the abnormal vertebrae did not separate properly. (Figure 3) On the x-ray these vertebra will look like triangles instead of rectangles. X-rays only show a two-dimensional representation of what is really a three-dimensional problem. The abnormally shaped vertebra may cause a wedge in the front, back, or either side, or a combination, tilting the spine at that level. Pediatric spine surgeons often use descriptive terminology to designate how much growth potential may be in the congenital anomaly. The term "fully segmented" indicates that there is a growth plate and a disk on both the top and bottom of the abnormal vertebra. "Semi-segmented hemi vertebrae" have a disk and growth plate either above or below. "Non-segmented hemi vertebrae" are fused to the vertebra above and below. Since non-segmented hemi vertebrae have no growth plates, the curves they cause are much less likely to progress than those due to semi-segmented hemi vertebrae, which are less likely to progress than a fully segmented hemi vertebra. A "block vertebra" means that there is a missing disk space. Block vertebrae essentially have no growth potential and therefore rarely cause a progressive deformity.
In the thoracic (chest) part of the spine, congenital anomalies of the ribs often correspond with congenital anomalies of the vertebra. For example, an extra thoracic vertebra might attach to an extra rib. Vertebrae that are connected together may be associated with ribs that are connected together. The anomalies of the ribs and vertebrae are not always identical, but are often similar. A child with congenital spine anomalies often has more than one. This may be a congenital failure of formation on both the right and left sides of the spine or several grouped together or a mix of failure of formation and segmentation.

After the history and physical examination, the next step in evaluating congenital scoliosis is obtaining x-rays. X-rays of the neck should be taken to look for abnormal vertebrae in this region. The three-dimensional structure of the congenital anomaly may be best visualized on a CT scan with reconstruction (this study is usually done as part of a preoperative planning) (Figure 4). An MRI is very valuable to characterize the congenital anomaly and to be certain that there are no associated anomalies of the spinal cord. In children younger than 3 months (before the vertebrae ossify and harden), an ultrasound examination can scan the spinal cord for abnormalities without the need for sedation. The evaluation of the congenital spine will also include an assessment of the kidneys and the heart Because the kidneys and heart are formed at the same time as the vertebrae, children with congenital scoliosis have a 25% chance of having an anomaly in the urologic system (kidneys, bladder) or a 10% chance in the cardiac system. The child's limbs should be examined for any musculoskeletal abnormalities, such as a clubfoot or malformed hand/arm.
When your child's congenital spine anomaly is first diagnosed, no one will know exactly how much the spine deformity will progress as the child grows. There are some clues, however. Anomalies in the thoracic spine tend to worsen with growth of the patient. Multiple fully-segmented hemi vertebrae on the same side of the spine also tend to progress with growth. A hemi vertebra opposite a set of fused vertebrae is the most likely combination to progress as the child grows. Because the most rapid period of spinal growth is in the first 5 years of life, and then at adolescence, these are the two times when the congenital curvature must be monitored most closely.
Observation is usually the first method of treatment for a young child with a spinal deformity. The physician will first need to determine if the curvature is progressing or worsening. Some children will have a curvature of their spine that is stable and unchanging, whereas other children will have a curve that relentlessly progresses. Just because the pediatric spine surgeon is "observing" your child does not mean that he/she is not treating them. During this period of time, not only will your child's doctor look for changes in the curve, but they will probably order some special tests to evaluate further the child's condition and have you see some other doctors.
Your pediatric spine surgeon will probably want to see your child every four to six months and have new x-rays made. They will then measure the curves and compare them with the previously made films. The doctor will probably continue to observe your child's curves as long as there is no drastic increase in the size of the curve. In some rare cases, the curve improves or even resolves. If your pediatric spine surgeon documents progression of the curve, though, a different form of treatment will need to be instituted. The surgeon will probably want to obtain bending radiographs of the spine to assess flexibility and help determine the next course of treatment.
If the curve is progressive, and your child is still growing, the doctor will inform the parent of the lack of evidence that a brace or cast can prevent progression of a congenital scoliosis.
An operation is sometimes necessary to address spinal deformity in the young child, and the decision to do these procedures is based on many factors. If the child's curve has shown progression despite bracing or casting, something will need to be done. The dilemma faced by the surgeon is how to stop the progression of a curve without adversely affecting future growth. Sometimes this is unavoidable, as most operations work by stopping abnormal spinal growth in a procedure called spinal fusion.
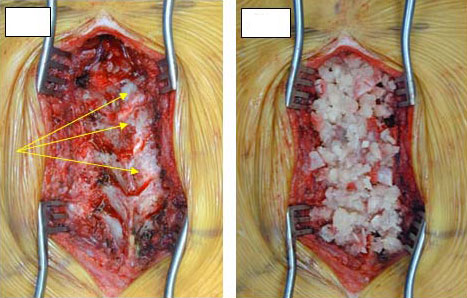
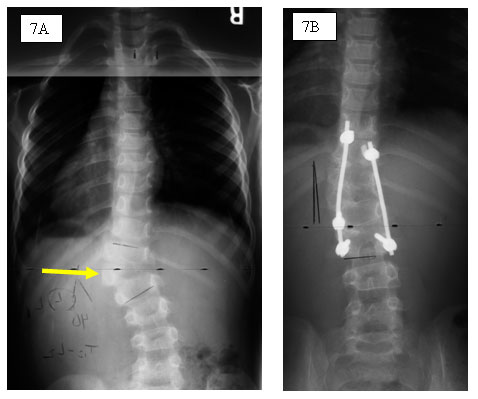
Spinal fusion is a procedure performed to stop growth of the spine. It can be done from the back (posterior) or through the chest (anterior) or both. The joints of the spine are removed, and a bone graft is placed; when the bone heals there will be a fusion mass, or one solid piece of bone (Figure 1). The goal is for the many vertebrae of the spine to become one segment and stop growing crooked. In situ fusion means that the curve will be fused "where it is" with little or no correction of the spine. Sometimes instrumentation (rods, hooks, and screws) may be placed to help straighten the spine slightly and act as an internal brace for the bone graft that will form the fusion mass. When implants are not used, usually in young children, the child may need to wear a brace or cast following the operation.
The goal of an in situ spinal fusion is to address the problem early, before it becomes a serious deformity. For example, if a pediatric spine surgeon sees a child with a 40o curve that has a poor prognosis (high chance to progress); he/she may elect to perform a limited spinal fusion to prevent the curve from getting any bigger. It is generally a safer procedure than those that correct the curvature of the spine. The results of a procedure to correct the curve at a young age can be unpredictable, as continued growth of the spine in other areas can cause the curve to progress or rotate (twist around).
This surgical procedure is aimed at stopping abnormal growth on one side of the spine with the hope that continued growth on the other side will result in correction of the curve over time. Every curve has a concave and convex side. If the growth centers are removed and spinal fusion is performed on the convex side, the concave side might continue to grow, possibly improving the curve. As noted, these procedures can be unpredictable in young children with abnormal vertebrae in their back.
Some young children with scoliosis may have abnormally shaped vertebrae in their back that causes the curve. Normal vertebrae are shaped like rectangles. A hemi vertebra is shaped like a triangle or trapezoid. When this hemi vertebra is located at the bottom of the spine it can tilt the base of the spine and cause the child lean to one side. In other parts of the spine, depending on the number of hemi vertebrae present, severe deformity can develop. Depending on your child's situation, this hemi vertebra may be removed from the front, back, or both parts of the spine. Once the hemi vertebra is removed the vertebrae above and below it are fused together, often with instrumentation. Most children will wear a brace or cast after the operation until the spine heals. This operation has inherent risks involved; including bleeding and neurologic injury, but good spinal correction is often achieved.
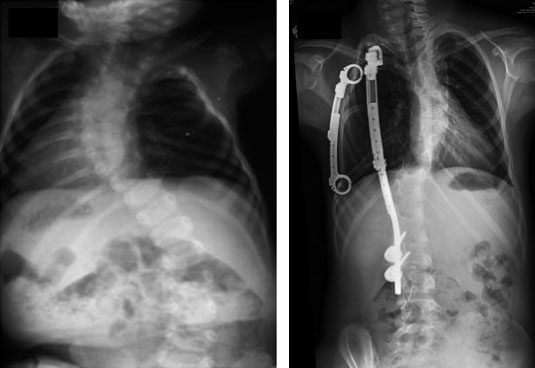
Most operations that address spinal deformity in the young child work by stopping growth. This may have unfavorable effects on growth of the thorax, lung development, and size of the trunk. The theory of the growing rod operation is to allow for continued controlled growth of the spine. This is done through the back of the spine. In general, the curve is spanned by one or two rods under the skin to avoid damaging the growth tissues of the spine. The rods are then attached to the spine above and below the curve with hooks or screws. The curve can usually be corrected by fifty percent at the time of the first operation. The child then returns every six months to have the rods "lengthened" approximately one centimeter to keep up with the child's growth. This is usually an outpatient procedure performed through a small incision. Most children will have to wear a brace to protect the instrumentation. When the child becomes older and the spine has grown, the doctor will remove the instrumentation and perform a formal spinal fusion operation. In the past, this procedure had a very high complication rate, most of which were related to the instrumentation (hook dislodgement, rod breakage). Newer techniques are more promising but treatment with growing rods remains a long, difficult therapy for the child.
Thoracic insufficiency syndrome, a newly characterized disease, is defined as the inability of the thorax to support normal respiration or lung growth. The thorax, which includes the spine, the rib cage, and the sternum, is the engine of respiration. It must have adequate volume for the underlying lungs to grow and it must be able to change that volume for breathing (respiration) to occur.
Thoracic insufficiency syndrome plays a part in the development of a child in two distinct ways. The first is the inability to support normal respiration. A thorax in early stages of deformity from scoliosis or from fused or absent ribs may have a minor degree of inhibition of respiration and the patient may appear normal. As the deformity worsens, the respiration can become more labored with increase respiratory rate and the inability to keep up with playmates in play activities. When thoracic volume is severely decreased and the diaphragm is the sole source of respiratory effort, then children may need aides such as nasal oxygen, BiPap ( pressure mask delivering oxygen), or even ventilator support to maintain life sustaining oxygen levels in their blood. The second component of thoracic insufficiency syndrome is the inability of the thorax to support lung growth. Early in life, a small thorax may be adequate for an infant, but if the child grows without the thorax enlarging with normal growth sufficiently to accommodate adult size lungs, then by the time the patient becomes a teenager, the thorax that was adequate during early childhood is very inadequate for adult oxygenation needs.
In thoracic insufficiency syndrome, the three-dimensional deformity of the thorax can limit its important role as a respiratory engine. Diseases can affect the spine and rib cage in many different ways, but the common problems are deficiencies in thoracic volume, symmetry, and function.
Most of the work of breathing is accomplished by the work of the diaphragm muscle, which is the thin muscle at the base of the thorax underneath the lungs. When the diaphragm contracts, the volume of the thorax increases with the air brought into the lungs. When the diaphragm muscles relax, air is forced out of the lungs. Another important contribution to the act of breathing is the outward expansion of the chest wall itself from the many small muscles between the ribs. For the thorax to have optimal efficiency as a respiratory pump, it must have ideal volume for age, the ribs need to have a symmetrical shape in order for them to move properly, and the diaphragm muscle must be properly anchored at the base of the chest. In congenital scoliosis, there can be missing or fused ribs. When there is an absence of ribs, the underlying lung collapses inward with breathing without effectively expanding. In fused ribs and congenital scoliosis, the concave side of the curve usually contains a lung constricted by the fused ribs. Additional loss of thoracic volume may be seen in scoliosis when the curve rotates the spine into the chest on the convexity of the curve, often protruding deeper into the chest in a deformity called lordosis (sway back), flattening the chest with loss of thoracic volume. In this instance, the ribs cannot move well enough to contribute to respiration, and breathing becomes totally dependent on the diaphragm muscle. Increasing deformity of the thorax results in greater volume loss and may lead to respiratory problems to a point that a child may require oxygen or even ventilator support.
Recently, a new surgical technique termed "expansion thoracoplasties" with the vertical expandable prosthetic titanium rib (VEPTR or "titanium rib") device, have been approved by the FDA to treat the combined thoracic deformity (spine/rib cage) by enlarging the constricted chest and straightening the spine indirectly without a spine fusion. Vertical Expandable Prosthetic Titanium Rib (VEPTR) expansion thoracoplasty was recently approved by the Food and Drug Administration for treatment of thoracic insufficiency syndrome in skeletally immature patients. Thoracic insufficiency syndrome (TIS) is usually associated with uncommon three-dimensional deformities of both the spine and rib cage. Several types of VEPTR based expansion thoracoplasties operations can be used for different types of deformities to gain chest volume for growth of the underlying lungs while indirectly correcting the scoliosis without spine fusion. (Figure 6) VEPTR surgery is extensive, devices are placed under the scapula (shoulder blade) and are attached to the ribs near the neck and continue down to either the spine, or the ribs near the waist, this helps to stabilize the surgically expanded chest wall constriction (expansion thoracoplasty). To accommodate later growth, the devices are expanded twice a year in outpatient surgery through small incisions. Currently, there are a limited number of institutions offering VEPTR surgery. Your child's spine surgeon can advise whether your child's condition is appropriate for VEPTR treatment and provide referral information, if needed. Some centers are using the VEPTR device as a means to straighten the spine indirectly via the ribs and chest wall.
Definitive spinal fusion is performed to stop growth of the spine and thus achieve permanent correction. This treatment becomes appropriate when the patient has demonstrated significant evidence of progression of the congenital scoliosis.
Posterior fusion provides permanent stabilization in the corrected position and is achieved by removing the joints between the vertebrae to be fused, usually all the vertebrae which are involved in the curve. Bone graft - either from the pelvis, ribs, or from the bone bank (allograft) - is placed in each joint space which has been removed. Over time (4-6 months), the graft incorporates to the vertebral bone, and the operated portion of the spine heals into a solid block of bone which cannot bend, thus eliminating further progression of the curve. Typically in a child who has reached an appropriate age for definitive fusion, instrumentation will also be placed when the fusion is performed. The instrumentation rigidly fixes the spine internally, so that the corrected position is carefully preserved while the fusion takes place over the 4-6 month period. This rigid fixation is achieved by screws, hooks, and wires ("anchors") attached to the spine, usually at multiple sites along the curve, and then rods are attached to the anchors to stiffen the entire area (Figure 1). Depending on the flexibility of the curve and any preceding treatment (such as traction), there may be additional correction of the deformity achieved by the application of the instrumentation. However, the primary goal of the surgery is to stop the curve from progressing further, and thus be the definitive stabilization - additional correction is an added benefit but not the primary concern. Often the patient does not need any further external immobilization (cast or brace) if the internal fixation device is felt to be adequate at the time of surgery.
Upon skeletal maturation, it is anticipated that most mild congenital scoliotic curves will not progress or be associated with back pain in adulthood.