

Low back pain is a common complaint among people who seek medical attention. It may originate from different sources in the back or pelvis. The SI joint (articulation of pelvic bone with the sacrum) has been recognized as a common source of sciatic pain since over hundred years ago especially before knowing intervertebral disc as a source of leg pain.
About 15% to 30 % of patients with LBP have SI joint as the pain source and up to 40% may develop such problem after back surgery with fusion of vertebrae together especially after longer fusions to the pelvis. This has been confirmed by an observational long-term study. This joint may become painful after pelvic injury, direct trauma to the joint, repeated micro-trauma, after pregnancy or in some rare joint diseases.
Considering common occurrence and lower quality of life following such problem, spine surgeons should be familiar with diagnosis and treatment of SI joint dysfunction in patients with LBP especially those who undergo fusion. Usually this includes a through history and physical examination, imaging and injection studies, and appropriate treatment.
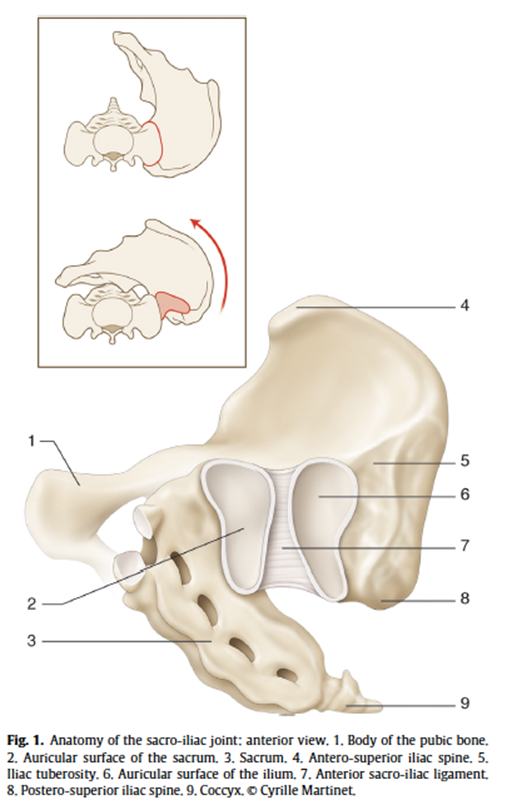
The SI joint is a complex joint which includes both cartilage and strong ligaments to transfer loads from the spine to the pelvis and helps childbearing in females. It has reach innervation from the nearby nerve plexus which makes it an important potential pain generator. It has a slight motion which is along its transverse axis (fig 1).
Among different causes of LBP which includes diseases of the spine and other areas like hip joint, sacroiliac joint problems must be considered by treating physician. According to a study in 289 patients with the complaint of LBP, 65% had problem just in the spine. 17.5% had combination of spine and hip or SI joint problems. They found up to 25% of patient with LBP may have a problem in the hip or SI joint.
The characteristic pain pattern is felt over the medial and distal part of the buttock and groin and lower limb. There may be a vague radicular pain in the leg which may be worsened when sitting on a hard surface for long time, walking upstairs or changing from sitting to standing position and vice versa (fig 2). A complete examination of the lower back, hip and neurological system must be done, and, in some cases, appropriate Lab tests must be done.
There are many physical exam maneuvers to elicit pain in the SI joint (fig 3). Although these tests are not specific or sensitive, if several tests (more than three) are positive this will be more valuable for diagnosis of SI pathology. In some cases, a needle injection done under image control serves both for diagnostic and treatment purposes.
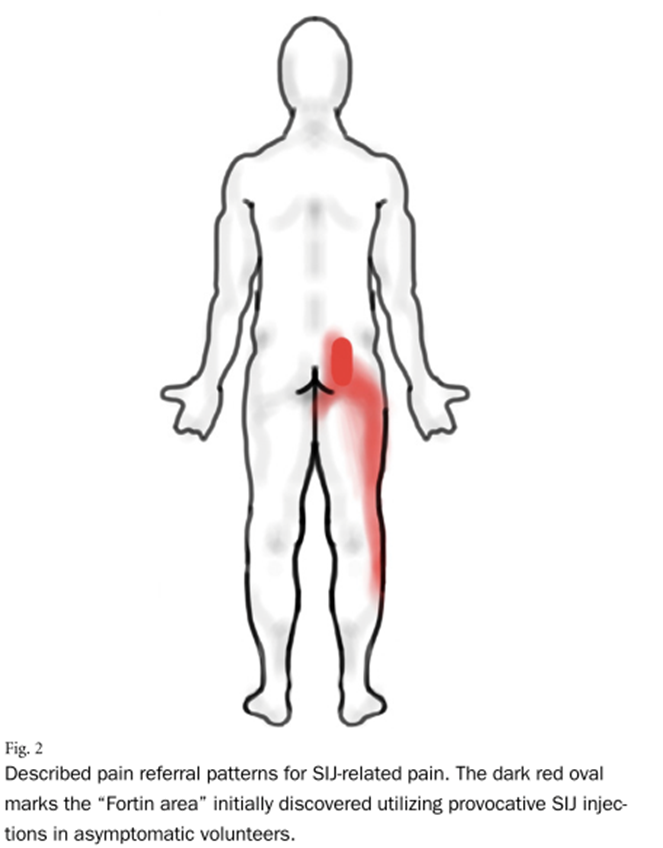
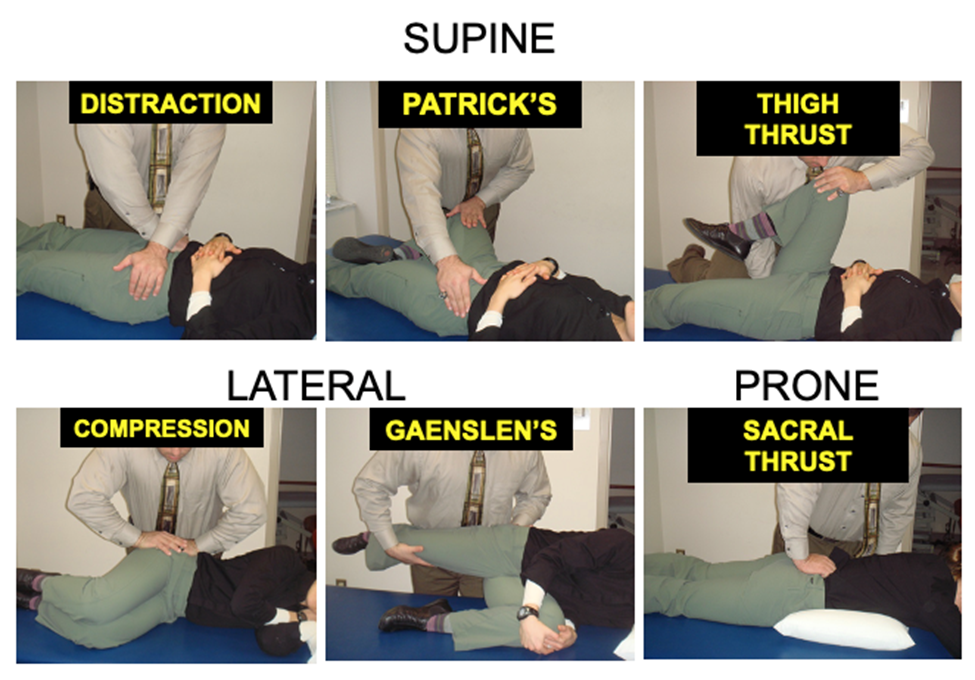
Figure 3. Physical exam maneuvers for diagnosis of SI joint dysfunction. 3 or greater positive tests indicates a significantly increased sensitivity and specificity.
Imaging studies are not helpful for diagnosis of SI problem; however, they are useful to find other sources of pain. It must be considered that there is common to find abnormalities in MRI in people without symptoms. Imaging may be helpful to find severe problems like fracture, infection, or tumor as the source of SI joint pain.
Pain relief after local anesthetic injection in the joint is considered the gold standard to confirm SI joint as a source of pain. Usually this is done under image control by an expert physician (fig 4). It should reduce the pain at least 50 to 75% from the baseline to be considered positive. Some authors advice two injections for confirmation and there are recommendations on the amount and type of anesthetics to be injected.
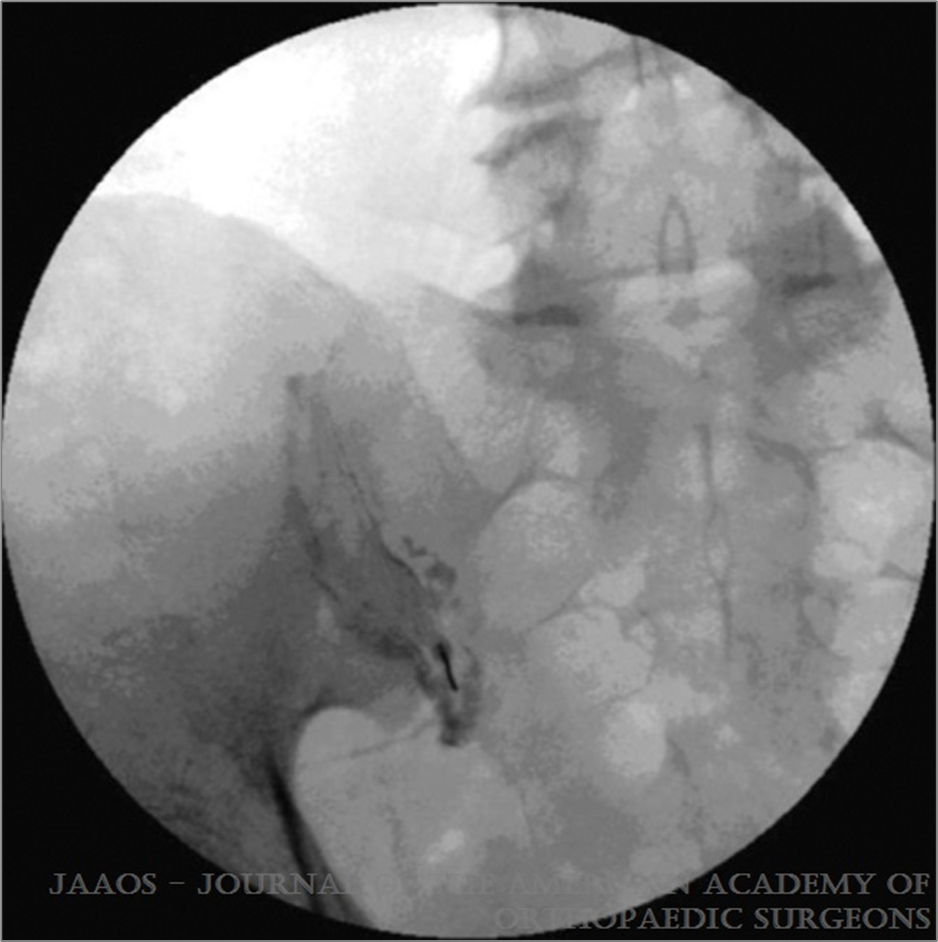
Figure 4. Diagnostic SI joint injection using fluoroscopic guidance.
Nonsurgical Management
Usually treatment with local ice, reducing activities and NSAIDs can be enough to avoid more intensive treatments. There is no evidence for efficacy of massage or manipulation. Pelvic belts may be used as a diagnostic test for short time. Neither electrotherapy nor rest has been shown to be beneficial. Acupuncture may be effective for SI joint pain during pregnancy. Despite conflicting results, there are some evidence that physical therapy may be effective to improve pain and function.
Intra-articular injection of steroids along with local anesthetic can be therapeutic along with the diagnostic injection. Radiofrequency Ablation (RFA) can be effective but more systemic reviews failed to show benefits when compared to other non-surgical treatments methods.
Surgical Management
In patients with persistent debilitating symptoms surgical treatments may be considered. Many operative techniques have been used for treating SI joint problems including open and limited open surgeries. There are mixed results following these procedures and controversy exists as the results of such approaches. In the recent decade new less invasive approaches have been developed to treat SI joint dysfunction (fig 5). Studies that are mainly sponsored by the industry show significant improvements in pain and functional results after two years and five years compared with non-operative treatment. Clearly these techniques have certain complications and must be done by physicians who are familiar with the anatomy and techniques.
The best comparative effectiveness study of non-surgical, RFA and MIS surgery in 2018 showed that the first two group did not improve while the MIS group achieved meaningful improvements in pain and disability which lasted for 6 years.
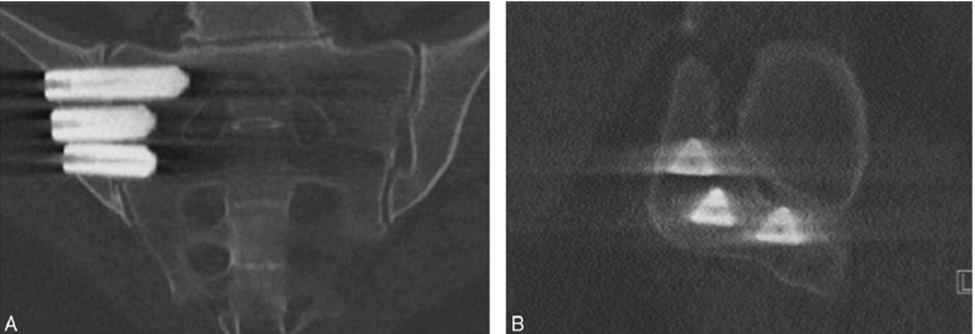
Figure 5. Minimally invasive SI joint fusion performed using triangular titanium implants.
A large percentage of patients with low back pain suffer from SI joint dysfunction. The diagnosis and treatment of SI joint dysfunction can be challenging to the clinician given the lack of specific physical exam or imaging findings related to patient complaints. However, when accurately diagnosed, treatment can markedly decrease pain, while increasing function and quality of life for this patient population.
Non-surgical measures, while not extensively studied, can be effective at improving symptoms and should be initiated first before surgery is considered. After confirmatory diagnostic sacroiliac joint injection in an appropriate surgical candidate, operative intervention with newer MIS techniques, has the potential to improve pain and disability compared to patients treated non-surgically. Long-term studies beyond five years are lacking, along with studies comparing the various minimally invasive options available.
Summary provided by Ruwan Ratnayake, MD; Fernando E. Silva, MD; David W. Polly, Jr., MD; Jean Charles Le Huec, MD, PhD; Frank Rand, MD; and Robert Eastlack, MD.