

Kyphosis is a larger-than-normal forward bend in the spine, most commonly in the upper back. In adults, 3 forms of kyphosis are seen:
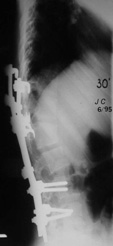
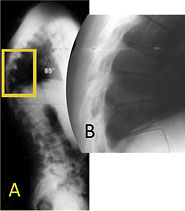
Post-traumatic kyphosis occurs most commonly in the mid- to lower-back. Kyphosis of this kind is typically found in patients with severe fractures and neurologic deficits such as quadriplegia or paraplegia. (See Figures 1A-1C)
One example of kyphosis is post-laminectomy kyphosis. In rare instances, the spine will develop a forward bend after a common procedure (laminectomy) used to treat spinal stenosis (pinched nerves) in adults – especially if many levels are decompressed.


Progressive kyphosis can develop when there is major spine injury. This type of kyphosis can result in chronic, disabling pain:
Goals of treatment for kyphosis includes curve correction, spine stabilization, pain alleviation, and improved neurologic function. The treatments shown below do not necessarily take into account the kyphosis patient who has osteoporosis. Numerous medications—e.g., Calcitonin, Forteo (teriparatide)—are now available; while they may decrease the pain, they cannot correct kyphosis. Current treatment options include:
If these conservative measures do not help, surgery may be necessary to control pain and improve curvature or decompress nerve roots. Posterior spinal fusion and instrumentation alone is often used to treat more flexible curvatures. Fixed curvatures often require more complex surgery.
Age-associated hyperkyphosis is a pronounced forward bend in the upper spine found in older adults. Sometimes called Dowager's hump or gibbus deformity, this type of kyphosis makes mobility difficult and increases the risk of falls and fractures. Hyperkyphosis can stem from a number of spinal conditions, like osteoporosis, muscle weakness, degenerative disc disease, and vertebral fractures, or a combination of these.
Standing x-rays are typically used to assess hyperkyphosis. Elderly patients, however, can be x-rayed lying on their backs. Using the x-ray, the physician will measure the degree of the forward-bending angle to determine the severity of kyphosis.
If these conservative measures do not help, surgery may be necessary to control pain and improve curvature or decompress nerve roots.
Scheuremann's kyphosis is a structural kyphosis that typically develops during adolescence, causing the kyphotic spine to become rigid, and sometimes progresses into adulthood. In the spines of these patients, the front sections of the vertebrae grow more slowly than the back sections. Instead of normal and rectangular with ideal alignment, the vertebrae are wedge-shaped and cause misalignment (Figures 1 and 2). The abnormal kyphosis is best viewed from the side in the forward-bending position where a sharp, angular abnormal kyphosis is clearly visible.
If kyphosis has become severe (greater than 80 - 90°) and causes frequent back pain, surgical treatment may be recommended. Surgery provides significant correction without the need for postoperative bracing. Pedicle screws are placed, 2 per vertebra, and connected with 2 rods. This process promotes gentle straightening of the spine. Most surgeries are performed from the back; however, some physicians recommend additional surgery on the front of the spine. Patients are usually able to return to normal daily activities within 4 to 6 months following surgery.
Moderately flexible curves often straighten simply from lying face down; however, rigid curves may require surgical intervention. The Smith-Peterson osteotomy involves cutting the bone in the back of the spine that connect the facet joints. The removal of this bone and the joints allows the spine to move backwards into extension or more of an upright position. This type of osteotomy is commonly performed during the surgical treatment of Schuermann's kyphosis.