Coding Corner

Barton L. Sachs, MD, MBA, CPE
2017-18 Coding Committee Chair
Accurate Clinical Documentation Integrity (CDI) Helps Advance Reportable Clinical Quality and Financial Reimbursement
Why CDI?
Clinical documentation integrity (CDI) and coding are not taught in medical school; therefore many physicians have no idea what CDI means and why it is important to them. But it is! Due to changes in reimbursement, increased scrutiny by third party payers, and most importantly the emphasis on all providers and hospitals to provide measureable quality patient care, CDI programs were developed. Physicians are not taught how to complete inpatient documentation in order to correctly assign codes and physician billing in the past has not required a great deal of specificity.
What is clinical documentation?
Clinical documentation is the accurate record of diagnoses made, symptoms observed, treatment procedure planned and executed, the care provided, the outcome of the treatment, and clinical assessment of the entire treatment process. Good clinical documentation will improve communication and identify further comorbid conditions that are evaluated, monitored or treated or add to resource utilization or increase length of stay during the hospitalization or present on admission (POA). In addition, good clinical documentation will validate the level of care the provider and hospital has provided to the patient and show compliance with quality and safety guidelines.
It is really all about quality!
The quality and specificity of a physician’s documentation is the key to accurate coding.
A hospital’s complete and accurate coded data is used for:
- Improved quality of patient care
- Accurate patient safety indicators
- Decision making on healthcare policies
- Optimizing resource utilization
- Identifying and reducing medical errors
- Value-based purchasing
- Clinical research and/or studies
- Consumer decision making
- National quality scoring and ranking
- Improving mortality ranking
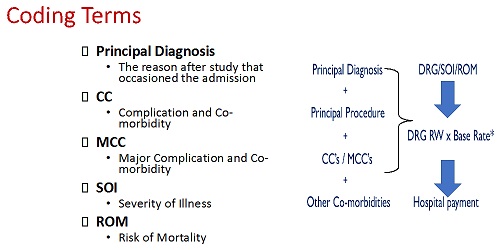
Example of coding terms that should be included when physicians submit coding.
How does CMS feel about CDI Programs?
“The [IPPS] documentation and coding adjustment was developed based on the recognition that the MSâ€DRGs, by better accounting for severity of illness … would encourage hospitals to ensure they had fully and accurately documented and coded all patient diagnoses and procedures consistent with the medical record in order to garner the maximum IPPS payment available under the MSâ€DRG system.” Source: CMS 2009 IPPS 73 Fed. Reg. 48448, Aug. 19, 2008
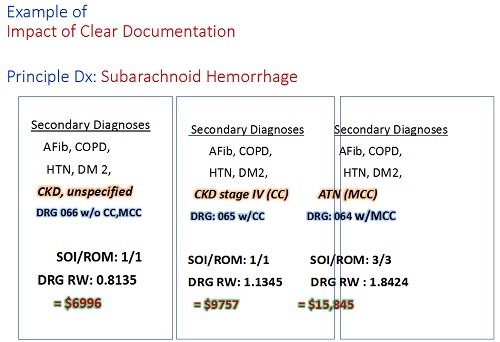
Example of how CDI alternatives will drastically affect reimbursement for clinical care.
Two statements from the Federal Register regarding CMS and accurate coding:
“We highly encourage physicians and hospitals to work together to use the most specific codes that describe their patients’ conditions. Such an effort will not only result in more accurate payment by Medicare but will provide better information on the incidence of this disease in the Medicare patient population.” Source: Federal Register, Vol. 72, No. 162, Wed. Aug. 22, 2007, Rules and Regulations, pp. 47180—47181.
“We do not believe there is anything inappropriate, unethical or otherwise wrong with hospitals taking full advantage of coding opportunities to maximize Medicare payment that is supported by documentation in the medical record. We encourage hospitals to engage in complete and accurate coding.” Source: Federal Register, Vol. 72, No. 162, Wed. Aug. 22, 2007, Rules and Regulations, pp. 47180–47181.
Summary
If one emphasizes the importance of having a high quality medical record, then the above objectives will be met and the appropriate reimbursement will follow!
This is the final anticipated Coding Committee article. We hope we have served you well with your coding needs these past years.
2017-2018 Committee
Chair: Barton L. Sachs Committee: Mathew D. Hepler, Past Chair, Advisory; William K. Koeck (C); Kathryn McCarthy Mullooly (C); Matthew E. Oetgen (C); Michael S. Chang; Walaa Elassuity; R. Dale Blasier, Advisory; John Frino



