Dear SRS members,
The past two years, we have taken a strategic look at all the work we are doing in education, communication, diversity, patient outreach and of course, research. As we have continued this work, we have found some obvious opportunities to redirect content and work in a more productive manner.
One of these areas is the quarterly members-only newsletter. After in-depth analysis of readership, content, and committee submissions, the SRS Board of Directors determined it no longer meets the strategic communication goals of the society for more robust, more timely communication of programs and initiatives.
We found that the low level of engagement, compared to the amount of time and work for our member committees and SRS staff was unequal. So, the Board of Directors made the decision at the IMAST Board meeting to cease publication as of the March 2022 issue. Committee reports and member-only information are now incorporated in the members-only section of the e-newsletter, the "Spinal Column."
In addition, we will produce a yearly, interactive, online Annual Report that will highlight the full year of committee achievements and SRS successes.
We value member communication highly. We plan to continue fine tuning and updating our options to deliver the most relevant content in the best possible format in the future. That includes investing in new platforms like an online, interactive Annual Report, the Scoliosis Dialogues podcast and a new membership website.
We look forward to another great year of SRS growing and expanding as the premier, international research society.
Sincerely,
.jpg)
Christopher Shaffrey, MD
SRS President
Read more »

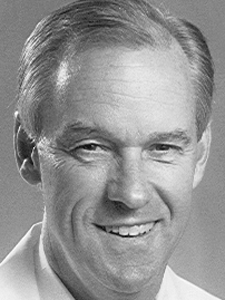
Preston Phillips, MD
As most of us have heard, SRS member Dr. Preston Phillips was shot and killed in Warren Clinic on South Yale Avenue in Tulsa, Oklahoma on June 1, 2022.
As I contemplated writing this obituary, I thought of the enormity of good that can be done by one professional in our field. Among our membership we have some of the leading practitioners in the field of spinal deformity. Our collective knowledge has spearheaded advances in spinal surgery all over the world. Dr. Phillips represented that drive for knowledge in every area of his career.
In just four years at Emory University, Dr. Preston graduated with a bachelor's degree in theology, a bachelor's degree in chemistry and a master's in organic chemistry. 
After Emory, Dr. Phillips was accepted to Harvard Medical School and graduated with honors in 1992. He also completed fellowships at Beth Israel Deaconess Medical Center in Boston and Boston's Children's Hospital.
According to his obituary from Harvard, he was the former team physician for the Tulsa Shock, part of the Women’s National Basketball Association. Phillips also participated in medical missions to Africa, organized by the Tulsa-based Light in the World Development Foundation.
In addition to being a standing member of SRS, he was a Fellow of the American Orthopedic Association (AOA), and American Academy of Orthopaedic Surgeons (AAOS). He was also a member of the J. Robert Gladden Orthopaedic Society (JRGOS).
AOA issued a statement after Dr. Preston’s death that sums up how we all feel as we move forward: “We will continue to care for our patients and embrace the oath we took as physicians. Although our hearts are heavy and our hands are weary, we will continue our service to others and never forget those who we have lost while in the line of duty.”
You can watch the celebration of life for Dr. Phillips here.
Read more »
Do you have an idea for an innovative topic for the 2023 IMAST program?
The IMAST Committee is accepting SRS member applications for IMAST Education Sessions from May 6, 2022, through June 3, 2022. Formats include Instructional Course Lectures, Debates, and Case Sessions. Alternative session formats for creative learning experiences also welcomed.
Educational content for IMAST should focus on innovative topics and surgical techniques, new spine technologies, and emerging practice challenges and solutions.
Submission requirements:
- Agenda
- Presenter list (SRS members strongly preferred)
- Rationale for topic timeliness, relevance, and innovation
- Description of educational needs addressed
- Description of patient care problems associated with this topic
- 2-4 quiz questions on priority learning outcomes
Contact the SRS Education Team at [email protected] with any questions.

IMAST, the Scoliosis Research Society’s (SRS) International Meeting on Advanced Spine Techniques, gathers leading spine surgeons, innovative research, and the most advanced spine technologies and techniques in an international forum. For three days, surgeons from around the world discuss, debate, and demonstrate new spine techniques to help each other improve patient care.
Read more »
by Craig Louer, MD
Scenario:
An adolescent patient elects to proceed with posterior spinal fusion (PSF) for AIS. The curve is classified pre-operatively as Lenke 1C-, characterized by a structural main thoracic curve with significant hypokyphosis; and, the clinical exam correlates with this sagittal plane disruption. The main thoracic (MT) coronal Cobb measures 55 degrees and it demonstrates reasonable flexibility in the coronal plane. This surgeon would not typically use posterior column (Ponte-style) osteotomies to improve correction for a main thoracic curve like this in isolation. However, in this particular case, a selective thoracic fusion is the chosen surgical approach and the surgeon hopes to maximize MT correction to better influence spontaneous lumbar curve correction.1 The surgeon uses this as justification to perform 5 apical Ponte osteotomies during the procedure. Surgery is complicated by intra-operative neuromonitoring alerts but ultimately no neurologic deficit is noted at wake-up test or final outcome. Desired correction is achieved, and patient has a routine post-operative course subsequently.
Afterwards, the surgeon considers the ethical underpinnings of the decisions made, including:
"How much increased surgical risk is tolerable for incremental gains in correction with uncertain influence on ultimate long-term outcomes?"
Or to phrase another way,
"If this patient suffered significant or irreversible neurologic deficit as a result of Ponte osteotomies, would the potential or realized gains of such a strategy be adequate justification?"
Discussion:
Although rarely do surgeons ask themselves these questions explicitly, they are nonetheless encountered and addressed by our routine decisions. Each of us has been honed during training and practice to be passable judges of relative risk and benefit. Every surgical indication considers relative risk and benefit of a procedure and whether this balance is "acceptable".
The topic of acceptable risk for Ponte osteotomies in AIS has been an area of internal debate for me as a young surgeon, as well as a public and sometimes fervent debate within our specialty. Ponte osteotomies are routinely performed for all curves in some practices, while in others it is a rarity only for extenuating circumstances.2 Controversial and sometimes opposing viewpoints have been presented during research podiums at national meetings, making the dichotomy in practice patterns relatively apparent. Why would a group of surgeons who seem to agree on the favorable benefits-to-risks ratio for a procedure like PSF for AIS have opposing viewpoints on the related procedure of Ponte osteotomies? Perhaps it is because we do not agree to the same set of facts like we do for PSF.
The Ponte osteotomy was developed in 1987 by Dr. Alberto Ponte of Rome, Italy. It was originally developed for kyphosis, but it has been noted more recently by its creator to have ability to correct coronal and rotational deformities in addition to sagittal deformity.3 Within the last decade there have been numerous reports of incorporating Ponte osteotomies into the PSF procedure for AIS, with general improvements in coronal, sagittal, and axial corrections compared to controls, though the studies are observational and the clinical significance of the modest improvements are debatable.4,5 One situation where these small changes in deformity characteristics may be clinically relevant is in the situation of a selective thoracic fusion where spontaneous lumbar curve correction appears to be influenced by the magnitude of coronal correction and, to a lesser degree, the kyphosis restoration.1
In other cases, it is speculated that restoration of thoracic kyphosis is the most essential component of deformity correction, as this kyphosis restoration may positively influence overall sagittal profile by allowing physiologic lumbar lordosis and reducing the presence of cervical kyphosis.6,7 Long-term follow-up may help determine whether these purported benefits will affect healthcare related quality of life, though there is sparse evidence of an immediate or mid-term advantage in outcomes attributable to Ponte osteotomies for AIS.
The performance of Ponte osteotomies has been associated with additional risks. In a large series of 2210 patients, Buckland et.al. reports a risk of realized neurologic complication to be quite low and similar between AIS groups undergoing PSF with Ponte Osteotomy (PO) or No PO (0.37% vs. 0.17%). Although no statistical difference in the manifested complications, there was a significantly increased rate of neuromonitoring alerts in the group undergoing POs (9.3% vs. 4.2%).8 Additional studies have substantiated that the risk of a neuromonitoring alert is increased if Ponte osteotomies are utilized.9 There are other potential risks with Ponte osteotomy use, including increased blood loss, operative time, and concern for wound issues if hematoma were to form.
Proponents of Ponte osteotomies would argue that PSF is a deformity correction operation, and the Ponte osteotomy is a powerful tool to help them best achieve maximum correction. These individuals recognize that it will cost them some time and may result in increased neuromonitoring alerts. However, they do not weigh the risk of neurologic injury to be significantly increased over baseline. Detractors of this practice would state that neuromonitoring alerts are a critical outcome meant to be avoided. These surgeons believe that they can accomplish their PSF goals of limiting future progression with a minimal risk operation and they perhaps don’t believe maximum radiographic correction in all three planes is a goal that warrants additional risk.
The other significant consideration that must be acknowledged is the impact of reimbursement in our decision-making. Many surgeons have compensation plans that are productivity-based, where at least part of their salary is determined by clinical productivity measured by work-RVUs (wRVU). The code for a single posterior column osteotomy (PCO) (thoracic-level CPT 22212) is worth 20.99 wRVU; a lumbar PCO is worth slightly more. In the current system, this means a single PCO would generate more wRVU than open treatment of femoral shaft fracture (CPT 27506, wRVU-19.65) and over 70% of the wRVU of a suboccipital and cervical decompression for Arnold-Chiari malformation (CPT 61343, wRVU 31.86). While additional levels of PCO don’t generate wRVUs quite as generously as the initial PCO (CPT 22216, wRVU 6.03), PCOs collectively have a large effect on the procedural charge and reimbursement.
While we assume (and hope) that there are very few surgeons who make decisions solely based on billing, the realities of reimbursement may subconsciously sway many more surgeons who understand the impact it has on their (or their hospital’s) bottom line. Cognitive dissonance can lead to rationalization to use PCOs for a medical indication, though the subconscious motivation is repayment. Any productivity-based surgeon who knows how they are reimbursed is subject to such bias. Pretending it does not exist would be naïve.
As for the solution to this ethical dilemma, unfortunately there is no clear answer. The well-known clinical ethical principles of beneficence and non-maleficence are at odds with many cases of surgical decision-making. With these two principles in conflict, determination of which should prevail would depend on weighing an individual surgeon’s interpretation of the data. The answer may vary for each surgeon or patient, with risks somewhat mitigated with more surgical experience or skill, or the benefits more pronounced in some patients where routine measures will not result in an acceptable outcome. As evidence evolves, new patients seek care, and we continue to change as individual surgeons, I submit that this decision should change in accordance. Do not be blind to your biases and subconscious motivations. Continued introspection and re-evaluation is essential in surgery. Ask yourself: “If a complication were to result from the performance of this Ponte osteotomy, would I still feel performing the procedure was necessary and was the best decision for this patient?” Also ask, “Would I make the same decision if payment were unaffected?” When these are answered in the affirmative, then your assessment favors the performance of a Ponte osteotomy.
1. Kluck D, Sullivan TB, Bastrom TP, Bartley CE, Yaszay B, Newton PO. Predictors of spontaneous lumbar curve correction in thoracic-only fusions: 3D analysis in AIS. Spine Deform. 2021;9(2):461-469. doi:10.1007/s43390-020-00231-0
2. Oetgen ME, Weinstein SL, Andras L, Shah S, Sucato DJ. What are Your Optimal Surgical Strategies for a Double Major Curve in Adolescent Idiopathic Scoliosis? 2020;2(1):28.
3. Ponte A, Orlando G, Siccardi GL. The True Ponte Osteotomy: By the One Who Developed It. Spine Deform. 2018;6(1):2-11. doi:10.1016/j.jspd.2017.06.006
4. Samdani AF, Bennett JT, Singla AR, et al. Do Ponte Osteotomies Enhance Correction in Adolescent Idiopathic Scoliosis? An Analysis of 191 Lenke 1A and 1B Curves. Spine Deform. 2015;3(5):483-488. doi:10.1016/j.jspd.2015.03.002
5. Shah SA, Dhawale AA, Oda JE, et al. Ponte Osteotomies With Pedicle Screw Instrumentation in the Treatment of Adolescent Idiopathic Scoliosis. Spine Deform. 2013;1(3):196-204. doi:10.1016/j.jspd.2013.03.002
6. Newton PO, Yaszay B, Upasani VV, et al. Preservation of Thoracic Kyphosis Is Critical to Maintain Lumbar Lordosis in the Surgical Treatment of Adolescent Idiopathic Scoliosis: Spine. 2010;35(14):1365-1370. doi:10.1097/BRS.0b013e3181dccd63
7. Feng J, Zhou J, Huang M, Xia P, Liu W. Clinical and radiological outcomes of the multilevel Ponte osteotomy with posterior selective segmental pedicle screw constructs to treat adolescent thoracic idiopathic scoliosis. J Orthop Surg. 2018;13(1):305. doi:10.1186/s13018-018-1001-0
8. Buckland AJ, Moon JY, Betz RR, et al. Ponte Osteotomies Increase the Risk of Neuromonitoring Alerts in Adolescent Idiopathic Scoliosis Correction Surgery. Spine. 2019;44(3):E175-E180. doi:10.1097/BRS.0000000000002784
9. Floccari LV, Poppino K, Greenhill DA, Sucato DJ. Ponte osteotomies in a matched series of large AIS curves increase surgical risk without improving outcomes. Spine Deform. 2021;9(5):1411-1418. doi:10.1007/s43390-021-00339-x
Read more »
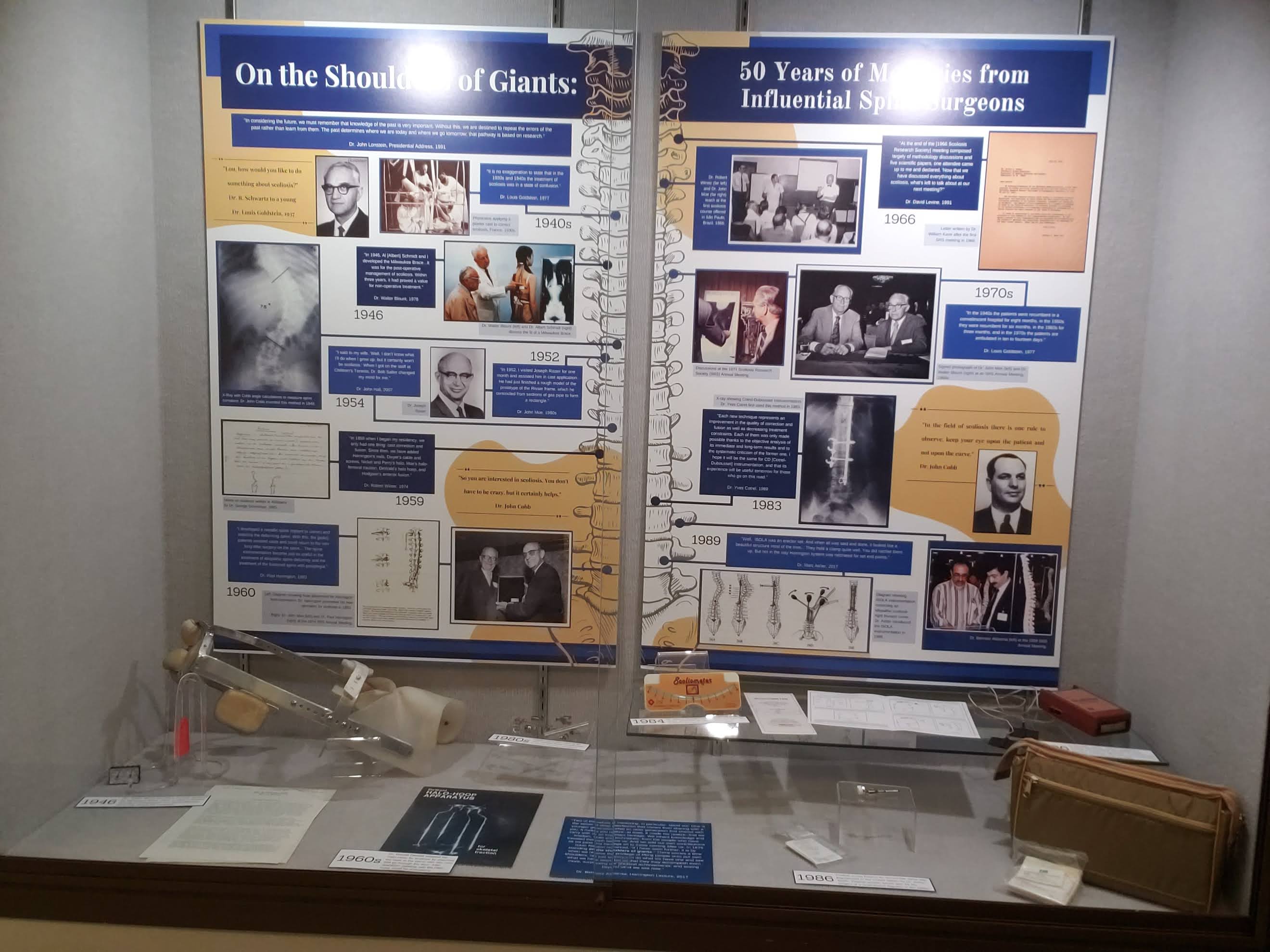
It was with great pleasure that the Historians of SRS visited the SRS archives in Kansas City. Along for the trip were Behrooz Akbarnia, George Thompson, Jay Shapiro, Rick Schwend, and Pat Kostial and of course the best of the SRS staff Laura Pizur. We met with the Archivists at KU med center where the Archives are housed along with the Harrington Archives. Good news in that a one-year position for an SRS Archivist will be filled this Fall.
Their job will be to better organize and arrange existing collection to make it easier find things in the collection for members and researchers. Long term goals are to make Archives more accessible in person and online.
SRS vice president Marinus de Kleuver was at University of Kansas Medical Center visiting and was able to stop in and see the Archives and the Harrington display as well as meeting with the Historians. We much appreciated his input and enthusiasm.
Seeing the displays is a must for all spine deformity surgeons. Knowing our history is vital for our future. Having the Archives allowed for documentation of spinal techniques that predated FDA rules allowing for the approval of new growing techniques and instrumentation as well as documenting use of pedicle instrumentation. As Historians we are working and looking for ways to make sure we preserve for the future todays and past accomplishments of spinal deformity surgery.
If interested in visiting or contributing to the Archives, please let any of us know.
Jay Shapiro, SRS Historian
Read more »

Claudio Villela Pedras, MD
Claudio Villela Pedras, MD, former head professor of Orthopedic Surgery at Federal University of Rio de Janeiro and former Chief of Spine Deformities at National Institute of Orthopedics and Traumatology, Rio de Janeiro, died January 30, 2017.
Dr. Pedras was native of Juiz de Fora, Minas Gerais, Brazil and moved to Rio de Janeiro to study Medicine at the Federal University of Rio de Janeiro. He began his professional career as Orthopedic Surgeon at Miguel Couto Hospital and Trauma Hospital in Rio de Janeiro. His former Chief, Dr. Nova Monteiro, seeing a need for spinal pathologies treatment, inspired him to do a fellowship with Professor John Moe.
Dr. Pedras with Edgar Dawson MD completed, the first John Moe Fellowship Program in Minneapolis in 1972. Returning to Rio de Janeiro, he was recruited to work at Miguel Couto Municipal Hospital and later at Trauma Hospital, today called INTO, the Spine Deformity Center.
Dr. Pedras was always ahead of his time, interested in new technologies and was a pioneer in less invasive procedures for spinal surgery in Brazil, performing the first video assisted thoracoscopic procedure for thoracolumbar fracture at the University Hospital of Rio de Janeiro in the early 90s.
Read more »

Davis W. Clark, MD
SRS member Davis W. Clark, MD died July 8, 2022, after brief illness at age of 86. He was born July 19, 1935, in West Springfield, MA. Dr. Clark attended University of Rochester, NY, where he earned a degree in Geological Engineering. After graduation he enlisted in the U.S. Navy. Dr. Clark left the Navy to enroll in medical school at the University of Rochester School of Medicine, graduating in 1967. He did his internship and orthopedic residency at Strong Memorial Hospital in Rochester.
After training, he moved to Concord, NH and founded Concord Orthopedics, PA on July 10, 1972, where he practiced for 50 years. He was a member of the SRS, NASS and served as an orthopedic board examiner.
Dr. Clark is survived by his wife of 38 years Sandra C. Clark, daughters Elizabeth G. Clark, Laura Mitchell, Deborah Hale, and his sons Davis W. Clark and Michael Hale.
Condolences may be left on his Legacy page.
Read more »
Voting will take place online in conjunction with the 57th Annual Meeting in Stockholm, Sweden on September 16, 2022. Information on how to vote will be provided closer to the voting period.
Vice President

Laurel C. Blakemore, MD
Communication Council Chair

Ron El-Hawary, MD
Fellowship Committee

Gregory M. Mundis Jr., MD
Directors At Large
 |
 |
 |
| Lindsay M. Andras, MD |
Firoz Miyanji, MD, FRCS |
Kota Watanabe, MD, PhD |
Thank you to the 2021-2022 Nominating Committee
 |
|
 |
|
| Muharram Yazici, MD, Chai |
Todd J. Albert, MD |
Peter O. Newton, MD |
|
 |
|
|
|
| Stefan Parent, MD |
David W. Polly, Jr. MD |
|
|
Read more »
Kiyoshi Kaneda, MD
It is with sadness we report that Professor Kiyoshi Kaneda passed away on October 9, 2022. He was 86 years old.
Professor Kaneda was born in Fukushima Prefecture on September 7, 1936. He studied medicine at Hokkaido University School of Medicine, Sapporo, Japan. After graduating medical school in 1962 and completion of internship at Kyoto University he did his residency in orthopaedic surgery at Hokkaido University.
In 1973 he became a visiting clinical fellow with John E. Hall, MD at the Children Hospital, Harvard Medical School in Boston, Massachusetts. In 1974 he was a visiting clinical fellow with John Moe, MD and Robert B. Winter, MD at the Twin Cities Scoliosis Center, Minneapolis, Minnesota.
Upon returning to Sapporo in 1976, Professor Kaneda was appointed Associate Professor in the Department of Orthopedic Surgery, Hokkaido University School of Medicine. He devoted his career to scoliosis and spine surgery. In the early 1980’s, he developed a new dual rod anterior spinal fixation system (“Kaneda device”). In 1986, Professor Kaneda was appointed Professor and Chairman of the Department of Orthopedic Surgery, Hokkaido University.
He and his spine fellows worked with Professor Manohar M. Panjabi and contributed significantly to spinal biomechanics research. Professor Kaneda became a member of the Scoliosis Research Society in 1983 and was an Emeritus Fellow at his passing. He was a member of ISSLS and served as its President from 1996-1997. He received the ISSLS Wiltse Lifetime Achievement Award in 2004 and the NASS Wiltse Award in 2011.
But Professor’s Kaneda’s greatest legacy may well not be on any plaque, award, or patent filing. Professor Kaneda’s great and most enduring contribution to spine surgery is his program for promoting the exchange of information and training between surgeons in Japan and the rest of the world.
Read more »

Jay Shapiro, MD
Historian
The Historical Committee is pleased to announce our new archivist for the SRS Archives, Katie Dold.
Over the next year she will be responsible for cataloging and updating our collection with the long term plan to make more of the archived material available on the SRS website.
Katie graduated with her Master’s Degree in Library Science from Emporia State University and has experience working in both libraries and archives. Katie has fully immersed herself in the collection and the history of the SRS and we are excited to see what she will accomplish.
You can learn more about Katie’s accomplishments in her graduate school portfolio available here: https://emporia.digication.com/katie-dold
Read more »
Courtney W. Brown, MD
Dr. Courtney W. Brown, SRS Past President, passed away on November 15, 2022 after a brief illness with COVID-19. He was 87 years old. He is survived by his loving wife of 61 years, Ingrid, two sons and one daughter.
Dr. Brown was born on July 24, 1935, in New York City and spent his childhood and adolescence in Scarsdale, New York, and Washington D.C. He graduated from Scarsdale High School and then from Williams College in Williamstown, Massachusetts in 1956. He graduated from Columbia University College of Physicians and Surgeons in 1962 and did his internship and orthopaedic surgery residency at St. Luke’s Hospital in New York City (1962-1967).
During the Vietnam War, he served in the United States Air Force, first at Orlando Air Force Base and then a year at U-Tapao Air Force Base in Thailand. Upon his discharge he, Ingrid and the children traveled the West, visiting various cities and medical practices. They decided to make Colorado their home. He joined Lakewood Orthopedic Clinic in 1970, which later adopted the name Panorama Orthopedic and Spine Center when it moved to Golden, Colorado in 2000. He worked there for 40 years specializing in spine. Even though he officially retired in 2008, he continued to see patients, particularly those with traumatic spinal injuries at Craig Hospital.
He was a member of the American Academy of Orthopedic Surgeons (AAOS), the Association of Bone and Joint Surgeons (ABJS), and the Scoliosis Research Society (SRS). He became an active member of the SRS in 1976 and was an emeritus member at his death. He served as SRS President in 1999. He was also the AAOS member of the Board of Trustees to the Orthopaedic Research and Education Foundation (OREF).
He loved skiing and founded Blue River Trauma Society, which combined helicopter skiing in Canada with medical seminars. For several years he volunteered for the U.S. Ski Team. In the summers, his passion was golf – often in special and exotic places, such as the Lakewood Country Club and Troon Country Club in Scottsdale, Arizona. He was also a member of the SRS golf group and along with the late Ed Dawson and Bob Gaines, arranged the SRS golf tournament for many years.
In addition to his interest in golf and skiing, he was very much interested in education and was involved in the teaching of pedicle screw and thoracoscopic techniques. He was the first editor of SRS Surgical Techniques Manual as the Chair of the Instrumentation Committee. He was also one of the first Senior SRS Travelling Fellows.
Overall, he was an exceptional mentor and innovator. His dynamic personality, enthusiasm, and candor, as well as his kind and embracing character, will be sorely missed.
Written By: Behrooz A. Akbarnia, MD, Jay Shapiro, MD, George H. Thompson, MD
Read more »
Alberto Ponte, MD
On January 10, 2023, the Scoliosis Research Society (SRS) lost a prominent member. Alberto Ponte died in Amsterdam, Netherlands where he has lived since 2018. He was born in Graz, Austria on July 9, 1926. He was 96 years old. During his life he made many contributions to the evaluation and treatment of spinal deformities.
In 1953 Dr. Ponte received his medical degree from the University of Turin in Italy. He did his orthopedic residency at the University Hospital in Florence from 1953-1958. He spent two of those years as an exchange fellow in some of the most important orthopedic and trauma hospitals in Great Britain, Germany, Austria and Switzerland. He then in 1958 accepted a 1-year fellowship in scoliosis at the Hospital for Special Surgery in New York City with John Cobb, performing approximately 60 spinal surgeries. During this time, he also spent 7 months at the Bone Tumor Service of Memorial Hospital, New York. Dr. Ponte then furthered his spine deformity training by spending time with Walter Blount (Milwaukee, USA), John Moe (Minneapolis, USA) and Joe Risser (Pasadena, USA).
In 1960 Dr. Ponte returned to the University of Florence and founded the first spine ward in Italy. He performed scoliosis surgery using the techniques and methods he learned in the United States and became a Full Professor of Orthopedics in 1963. In 1968 he became corresponding member of SRS at the invitation of doctors Moe and Blount.
In 1969 he founded the first independent Spine Center in Italy (Pietra Ligure). That same year he described an underarm orthosis for lumbar and thoracolumbar scoliosis. He was the first to recognize hypotension as a cause of paraplegia after surgical correction of scoliosis (SRS Gothenburg 1973). Was the first in Italy to use hemodilution and autotransfusion (SRS Hong Kong 1977), and in 1977 was a founder, and for 2 years president of, GIS, the Italian Scoliosis Society.
In 1987 Dr. Ponte presented the Ponte Osteotomy at SICOT meeting in Munich (SRS Portland 1994) treating thoracic hyperkyphosis by shortening the posterior column and preserving the anterior column load sharing capacity. Which is now widely used to help correct various spine deformities. In 1989 he presented 3,025 hyperkyphotic patients treated in Pietra Ligure by Risser plaster casts at the SRS meeting in Amsterdam and the ESDS meeting in Rome. From 1976-2015 Dr Ponte treated 240 skeletally mature hyperkyphotic patients surgically, the first 56 with Harrington technique and last 184 from 1987 using the Ponte Osteotomy. By invitation of the Editor-in-Chief of the journal Spine Deformity he published “The True Ponte Osteotomy: By the One Who Developed It" (Spine Deformity Jan. 2018).
Dr. Ponte has served as visiting professor around the globe. He has attended 39 meetings of the SRS with several presentations and was presented with the SRS Lifetime Achievement Award in 2019.

He had many intimate collegial working relationships with several of the SRS’s founding and regular members. He is survived by his wife Ellen, son Roberto, daughter Stefania and granddaughter Beatrice.
Dr. Ponte will be remembered for his many contributions to improve the care of patients with spinal deformity, many of which have been the foundation for subsequent progress in our field.
Written by: Jay Shapiro, MD, George H. Thompson, MD, Behrooz A. Akbarnia, MD
Read more »

Rudolph A. Klassen, MD
Rudolph “Rudi” A. Klassen, MD died on November 15, 2022, at the age of 91 in Minneapolis, Minnesota. He was born in Winnipeg, Manitoba on January 30, 1931, to Russian Mennonite immigrants. He attended the United College in Winnipeg and then medical school at the University of Manitoba in Winnipeg. There he met Frieda and after graduation in 1956 they married. For the next 2 years he provided medical care to the Hutterite colonies in northern Alberta and Manitoba.
He was subsequently recruited as a general practitioner to Lamoure, North Dakota. In 1963 after 5 years, and developing an interest in Orthopedics, he started an orthopaedic residency at the University of Minnesota. He then developed an interest in pediatric orthopaedics, which led him to accept new challenges.
CARE International opened a children’s hospital in Tunis, Tunisia and Dr. Klassen, with his wife and 4 children, moved there for 2 years. While working in Tunis, he met Dr. Mark Coventry, the Chairman of Orthopaedics at Mayo Clinic, who recruited him to Rochester, Minnesota in 1969.
During his career Dr. Klassen published 20 peer-review articles according to PubMed.
Dr. Klassen practiced pediatric orthopedics and spine surgery as Associate Professor at the Mayo Clinic for 40 years. He was the consummate clinician and teacher recognized multiple times as Teacher of the Year by his residents.
He was a long standing member of the SRS and became a member emeritus in 1975. In 1996 he was named Mayo Physician of the Year. His advice to residents was frank but supportive, and he engaged them on a personal basis.
Written by: Jay Shapiro, MD
Read more »

Donald L. Gaines, MD
Donald L. Gaines, MD died on October 14, 2021 at 87 years of age.The SRS was just recently informed of his passing.
He was born in St. Louis, Missouri on October 12, 1934 and grew up in Camdenton, Missouri near the Lake of the Ozarks. He attended Itawamba Junior College on a baseball scholarship and transferred to and graduated from the University of Mississippi. e earned his medical degree from the University of Tennessee in 1958 and joined the US Air Force Reserve as a flight surgeon. Dr. Gaines completed his residency in orthopedic surgery at Vanderbilt University Hospital. He then did a spine deformity fellowship in Minneapolis, Minnesota. He returned to Nashville, Tennessee to private practice.
Dr. Gaines was a long standing member of the SRS and became an emeritus fellow in 1972.
He was chief of staff at Donelson Hospital and subsequently at Summit Hospital until his retirement in 1999. During his career he published two studies according to PubMed. He was a member of the Tennessee Orthopedic Society, Nashville Academy of Medicine, and the Davidson County Medical Society.
He was a well respected member of orthopaedics in Tennessee and his community.
Written by: Jay Shapiro, MD
Read more »

Thomas I. Lowry, MD
Thomas Irvin “Tim” Lowry died on August 1, 2020. The SRS was just recently notified of his passing. He was born in Laredo, Texas the youngest of 5 children to a medical family, both parents, grandfather and great grandfather were physicians.
Dr. Lowry entered Baylor University at 16 years of age. After graduating in only 3 years, he entered Baylor College of Medicine. After graduation he began an internship and residency in orthopedic surgery at the same institution. His training was interrupted by service in the US Army from 1962-1963 as chief of surgery at a MASH unit in peacetime Korea.
After the Army, Dr. Lowry returned to Houston, Texas to complete his residency. He continued his training for 6 months with Dr. Paul Harrington in spine deformity surgery. After spending 3 more months training in Florence, Italy and Edinburgh, Scotland he settled in Austin, Texas to practice spine surgery and joined the Austin Orthopedic Clinic. He became an active member of the SRS in 1973 and later an emeritus member. He was also member of the Travis County Medical Society and served on its ethics committee.
Written by: Jay Shapiro, MD
Read more »
Thomas I. Lowry, MD
Thomas Irvin “Tim” Lowry died on August 1, 2020. The SRS was just recently notified of his passing. He was born in Laredo, Texas the youngest of 5 children to a medical family, both parents, grandfather and great grandfather were physicians.
Dr. Lowry entered Baylor University at 16 years of age. After graduating in only 3 years, he entered Baylor College of Medicine. After graduation he began an internship and residency in orthopedic surgery at the same institution. His training was interrupted by service in the US Army from 1962-1963 as chief of surgery at a MASH unit in peacetime Korea.
After the Army, Dr. Lowry returned to Houston, Texas to complete his residency. He continued his training for 6 months with Dr. Paul Harrington in spine deformity surgery. After spending 3 more months training in Florence, Italy and Edinburgh, Scotland he settled in Austin, Texas to practice spine surgery and joined the Austin Orthopedic Clinic. He became an active member of the SRS in 1973 and later an emeritus member. He was also member of the Travis County Medical Society and served on its ethics committee.
Written by: Jay Shapiro, MD
Read more »

E. William (Butch) Schmitt Jr., MD
E. William (Butch) Schmitt Jr., MD, passed away on March 22, 2023. He was born on March 2,1937 in Jacksonville, Florida and was known as “Butch” throughout his life.
Dr. Schmitt is recognized for his contributions to Pediatric Orthopaedic Society of North America (POSNA) history. In 1974 he participated in the formation of the Pediatric Orthopedic Travel Group. The following year, the name was changed to The Pediatric Orthopedic Study Group (POSG). He became Secretary-Treasurer of POSG in 1975 and meeting co-chair and President in 1983. The Pediatric Orthopedic Society (POS) and POSG merged in 1983 to become POSNA.
He graduated high school at the age of 16 and went on to obtain a medical degree from Emory University. After his orthopaedic residency at Harvard University, he served in the United States Navy in the Vietnam War. Upon his return, he became a pediatric orthopaedic surgeon at Egleston, now known as Children's Healthcare of Atlanta. Dr. Schmitt treated children for more 40 years.
In addition to POSNA he was active in the American Academy of Orthopaedic Surgeons (AAOS) and the Scoliosis Research Society (SRS). He became an Emeritus Fellow of the SRS in 1976. During his career, he published six peer-reviewed articles. His major interests were trauma, scoliosis, spina bifida and cerebral palsy.
He has been a major contributor to the musculoskeletal care of children, as well as a leader in the field. He will be missed.
Written by: George H. Thompson, MD
Read more »

Reinhard A. W. Westphal, MD, PhD
Reinhard A. W. Westphal, MD, PhD died on September 27, 2022 at 94 years of age, at his home in Leland, Ohio.He was born in Stettin, Germany on May 26, 1928. After growing up in Stettin he was drafted into the German Army in 1944 at 16 years old. In 1945, he fled Russian captivity and resumed his education. He graduated from Albert Ludwig University in Freiburg, Germany with a PhD in medicine.
In 1957 he married Toni Baumgartner and they had two children. They moved to Columbus, Ohio where he did his orthopaedic surgery residency and entered private practice in the community. He was on the staff at Riverside Methodist Hospital, Ohio State University Hospital and Nationwide Children’s Hospital. Initially he focused on trauma, but later his main interest was scoliosis. He became an emeritus member of the SRS in 1981. During his career he was an active member of the Ohio Orthopaedic Society.
Written by: Jay Shapiro, MD and George H. Thompson, MD
Read more »

Denis Sakai, MD, Website Committee Chair
The Website committee had a very productive year and is pleased to announce the society’s move to a new SRS website is well underway.
Thanks to collaboration with the SRS staff and Northwoods -- a website building firm – we have approved Northwoods’ design recommendations and new sitemap structure that will help restructure the entirety of the SRS website.
The committee had been keeping track of the current state of the website by analyzing the website’s Weekly Reviews provided by the SRS Communication Team. After analyzing the reviews, the committee was tasked with preparing potential improvements to the current webpages. These improvements involved updating webpages with outdated medical knowledge/studies and enhancing Search Engine Optimization (SEO) by attaching keywords to webpages.
Patient information content on the website was the biggest target for these improvements, so over the next few months, the Website Committee will review and update the content as needed to help improve the patient user experiences.
At the 30th International Meeting on Spine Techniques in Dublin, the Website Committee presented a full build proposal from Northwoods to the Board of Directors for final review and approval and to begin the contracting process for the development planning of a new website. The Board approved the project, and the contract was initiated that week.
The new website is on schedule to partially to fully launched in September, 2023.
Thank you to all the committee members who worked on this project: Abhay Nene, MD, Cristina Sacramento Dominguez, MD, PhD; Carlos Abreu de Aguiar, MD; Ali A. Baaj, MD
Ryan E. Fitzgerald, MD; Toshiaki Kotani, MD, PhD; Joshua M. Pahys, MD; John C. Quinn, MD; Karl E. Rathjen, MD; Jay Shapiro, MD; Andrew J. Trontis, MD, MS and Shirvinda Wijesekera, MD
Read more »

Denis Sakai, MD, Website Committee Chair
The Website committee had a very productive year and is pleased to announce the society’s move to a new SRS website is well underway.
Thanks to collaboration with the SRS staff and Northwoods -- a website building firm – we have approved Northwoods’ design recommendations and new sitemap structure that will help restructure the entirety of the SRS website.
The committee had been keeping track of the current state of the website by analyzing the website’s Weekly Reviews provided by the SRS Communication Team. After analyzing the reviews, the committee was tasked with preparing potential improvements to the current webpages. These improvements involved updating webpages with outdated medical knowledge/studies and enhancing Search Engine Optimization (SEO) by attaching keywords to webpages.
Patient information content on the website was the biggest target for these improvements, so over the next few months, the Website Committee will review and update the content as needed to help improve the patient user experiences.
At the 30th International Meeting on Spine Techniques in Dublin, the Website Committee presented a full build proposal from Northwoods to the Board of Directors for final review and approval and to begin the contracting process for the development planning of a new website. The Board approved the project, and the contract was initiated that week.
The new website is on schedule to partially to fully launched in September, 2023.
Thank you to all the committee members who worked on this project: Abhay Nene, MD, Cristina Sacramento Dominguez, MD, PhD; Carlos Abreu de Aguiar, MD; Ali A. Baaj, MD
Ryan E. Fitzgerald, MD; Toshiaki Kotani, MD, PhD; Joshua M. Pahys, MD; John C. Quinn, MD; Karl E. Rathjen, MD; Jay Shapiro, MD; Andrew J. Trontis, MD, MS and Shirvinda Wijesekera, MD
Read more »
The archives of the Scoliosis Research Society are stored in the Clendening History of Medicine Library and Museum on the campus of the University of Kansas Medical Center.
The collection contains board of director and executive committee meeting minutes, financial records, leadership correspondence, historical documents, committee reports and records, video interviews, meeting and conference programs, photographs, SRS publications, pedicle screw litigation documents, artifacts, and more.
Digital copies of many of these items can be found on this website, along with abstracts of all papers presented at past SRS meetings. Members of the SRS are free to download copies of these materials, and higher resolution copies are available by request (contact [email protected]). Please credit the SRS Archives if these materials are used as part of a presentation or publication.
To search the Scoliosis Research Society collection, visit the finding aid here:
Collection: Scoliosis Research Society records | University of Kansas Medical Center Archives (lyrasistechnology.org)
This finding aid is a guide to help you find information and identify materials within the SRS collection. It outlines the arrangement of the Scoliosis Research Society records and describes the records in the collection. It also contains information about the history of the SRS, record access, the scope and content of the collection, and the archival history of the records.
You can search through the finding aid by browsing through the collection organization dropdown menu, which shows series, subseries, and folder information. You are also able to search the collection for specific topics or names.

Historical Display:
Archive Tour:
Read more »
Recently the SRS Historical Committee had the chance to travel to Kansas City, Kansas to conduct an interview with 2023 Lifetime Achievement Award winner, Douglas C. Burton, MD and to meet the SRS Archivist, Katie Dold, MLIS.

Pictured left to right: Richard M. Schwend, MD; Doug Burton, MD; Behrooz A. Akbarnia, MD; Jay Shapiro, MD and George H. Thompson, MD
The archives of the Scoliosis Research Society are stored in the Clendening History of Medicine Library and Museum on the campus of the University of Kansas Medical Center.
The collection contains historical documents such as board of director meeting minutes, committee reports, video interviews, meeting programs, photographs, SRS publications, artifacts, and more.
Digital copies of many of these items can be found on this website, along with abstracts of all papers presented at past SRS meetings. Members of the SRS are free to download copies of these materials, and are available by request (contact [email protected]). Please credit the SRS Archives if these materials are used as part of a presentation or publication.
To search the Scoliosis Research Society collection, visit the finding aid here:
Collection: Scoliosis Research Society records | University of Kansas Medical Center Archives (lyrasistechnology.org)
SRS Archivist, Katie Dold, MLIS has also created the historical displays pictured below.

Read more »

Ben E. Veraart, MD
March 19, 1931 - July 1, 2023
On July 1, 2023, Dr. Ben Veraart, passed away at the age of 92.
Ben Veraart trained as an orthopedic surgeon with Professor San Georgi in Nijmegen, the first professor of orthopedics in the Netherlands, and he became an SRS member in 1969.
He worked in OLVG hospital in Amsterdam, specializing in spine surgery. He was the founder of the multidisciplinary scoliosis team and one of the first practitioners in the Netherlands to perform scoliosis operations in children. From 1976 to 1979 Ben Veraart was president of the Dutch Orthopedic Society (NOV).
He had many international contacts within our society and was also an active member of SICOT, and local host of the SICOT World Congress in 1996, in Amsterdam.
Ben Veraart was an erudite person with a great interest in art and culture in addition to orthopedics. Among other things, he was regularly found in the concert hall in Amsterdam where he enjoyed the music.
Written by: Marinus de Kleuver, MD, PhD
Read more »
Paul W. Pavlov, MD, PhD
January 24, 1944 - March 20, 2023
Dr Paul Pavlov, MD, PhD passed away on March 20, 2023.
He is survived by his beloved wife Vera and his three children, Irina, Alexander, and Thomas.
Paul was born on January 24, 1944 in Sophia, Bulgaria. After his graduation in medicine from the University of Sophia, Bulgaria, Paul continued his medical career abroad. In 1969 he moved to The Netherlands, where he started his orthopedic training with Cornelis van Nes, the most renowned Dutch orthopedic surgeon of his time.
He developed his career as spine surgeon in the Sint Maartenskliniek, and under his leadership it became the premier orthopedic institution in the Netherlands.
Paul was a gifted and ingenious surgeon and, at the same time, an inspiring and demanding teacher. He was a mentor and role model for a whole generation of orthopedic surgeons—especially spine surgeons—in The Netherlands. He was one of the earliest Dutch SRS members, joining our society in 1993.
We remember Paul Pavlov as a visionary surgeon, innovator, teacher, and leader. He will be sorely missed by his many friends and colleagues.
Written by: Marinus de Kleuver, MD, PhD
Read more »
Paul W. Pavlov, MD, PhD
January 24, 1944 - March 20, 2023
Dr Paul Pavlov, MD, PhD passed away on March 20, 2023.
He is survived by his beloved wife Vera and his three children, Irina, Alexander, and Thomas.
Paul was born on January 24, 1944 in Sophia, Bulgaria. After his graduation in medicine from the University of Sophia, Bulgaria, Paul continued his medical career abroad. In 1969 he moved to The Netherlands, where he started his orthopedic training with Cornelis van Nes, the most renowned Dutch orthopedic surgeon of his time.
He developed his career as spine surgeon in the Sint Maartenskliniek, and under his leadership it became the premier orthopedic institution in the Netherlands.
Paul was a gifted and ingenious surgeon and, at the same time, an inspiring and demanding teacher. He was a mentor and role model for a whole generation of orthopedic surgeons—especially spine surgeons—in The Netherlands. He was one of the earliest Dutch SRS members, joining our society in 1993.
We remember Paul Pavlov as a visionary surgeon, innovator, teacher, and leader. He will be sorely missed by his many friends and colleagues.
Written by: Marinus de Kleuver, MD, PhD
Read more »
Paul W. Pavlov, MD, PhD
January 24, 1944 - March 20, 2023
Dr Paul Pavlov, MD, PhD passed away on March 20, 2023.
He is survived by his beloved wife Vera and his three children, Irina, Alexander, and Thomas.
Paul was born on January 24, 1944 in Sophia, Bulgaria. After his graduation in medicine from the University of Sophia, Bulgaria, Paul continued his medical career abroad. In 1969 he moved to The Netherlands, where he started his orthopedic training with Cornelis van Nes, the most renowned Dutch orthopedic surgeon of his time.
He developed his career as spine surgeon in the Sint Maartenskliniek, and under his leadership it became the premier orthopedic institution in the Netherlands.
Paul was a gifted and ingenious surgeon and, at the same time, an inspiring and demanding teacher. He was a mentor and role model for a whole generation of orthopedic surgeons—especially spine surgeons—in The Netherlands. He was one of the earliest Dutch SRS members, joining our society in 1993.
We remember Paul Pavlov as a visionary surgeon, innovator, teacher, and leader. He will be sorely missed by his many friends and colleagues.
Written by: Marinus de Kleuver, MD, PhD
Read more »

Raymond T. Morrissy, MD
1941-2023
Raymond T. Morrissy was a creative force shaping the future of pediatric orthopaedics. Raised in Chicago and then high school in West Palm Beach, he was fortunate to have early exposure to very thoughtful mentors, including Dr. Philip Lichtblau and Wood Lovell. He received his orthopaedic surgery training at the Harvard/Massachusetts General Hospital before it became the Harvard Combined Program. There he was influenced by Dr. William Harris to pursue a career of scientific inquiry. Dr. John Hall was his role model for the consummate pediatric orthopaedic surgeon. He was a fellow orthopaedic resident with Tony Herring, his lifelong colleague and friend.
Early in his career, Dr. Wood Lovell recruited Ray to be the Medical Director at the Atlanta Scottish Rite Hospital. With his superb leadership abilities, sharp wit and passion for excellence, Ray helped grow this small hospital, combined it with Egleston Children’s Hospital, to become the Children’s Healthcare of Atlanta. There he mentored and trained several generations of medical students, residents, and pediatric orthopaedic fellows. He probably is best known by current trainees as the editor of the textbook “Lovell and Winter’s Pediatric Orthopaedics” now in its 8th edition, as well as the “Atlas of Pediatric Orthopaedic Surgery. He also authored 48 pediatric orthopaedic articles as cited in PubMed. In 2007 he received the POSNA Distinguished Service Award.
Although he was best known for his breadth of knowledge in general pediatric orthopaedics, many of his clinical and research interests were related to the spine. He was a lifelong member of SRS since 1979. His research publications included brace treatment for scoliosis, scoliosis school screening, and torticollis. Many of his studies greatly increased our understanding of spine conditions and improved their treatment. A 1990 JBJS publication showed that intra-observer measurement error for Cobb angle was about 5 degree and interobserver error could be as high as 7 degrees. He taught us that allograft bone could be as effective and safe as autograft iliac crest, thus avoiding the morbidity of harvesting pelvic bone for generations of spine patients. He was well known for his NZ white rabbit studies which showed that it took both bacteremia and local trauma to cause metaphyseal osteomyelitis. This gave great insight for how young children may develop acute hematogenous spondylo-discitis.
As a mentor, creative thinker, and friend to many, Dr. Morrissy will be remembered and missed. Dr. Morrissy was preceded in death by his wife of many years, Lois. They had no children.
Written by: Richard M. Schwend, MD
Read more »

Fábio Ferri-de Barros, MD, MSc, FSBOT, FRCSC
March 11, 1971- July 19, 2023
On July 19th, 2023, SRS member Dr. Fábio Ferri-de-Barros passed away. Dr. Ferri-de-Barros was born in Sao Paulo, Brazil in 1971. He graduated from Fculdade de Ciencias Medicas da Soa Paulo with a M.D.
After finishing his Orthopedic training, he worked for 5 years in Ilhabela, Brazil. He also spent time in various locales as part of his training including the U.S., Australia, and Switzerland. In 2006 he moved to Toronto and completed a Pediatric Orthopedic and Spine Surgery Fellowship at the Hospiral for Sick Children at the University of Toronto as well as a master’s degree.
In 2010 he moved to Calgary and the Aberta Children’s Hospital, becoming one of two pediatric surgeons in the Calgary zone. Dr. Ferri-de-Barros was a clinical professor of Surgery at the Cummings School of Medicine of the University of Calgary.
He was President of the Canadian Pediatric Spine Society and an Honorary Fellow of the Brazilian Society of Pediatric Orthopedics. In 2017 he joined the SRS.
In the last months of his life, he suffered from severe depression and was taken by a tragic complication of this severe disease. The family feels it is important to break down the stigma associated with mental health disorders and would like to encourage anyone in distress to seek help just as they would for any other health issue.
He is survived by his wife Natalia Marangoni Ferri-de-Barros, children Matteo (Maria Luiza), Giovanna, and Nicolas.
Written by: Jay Shapiro, MD
Read more »



